Background
MedStar Health has always been committed to increasing access to behavioral health services as we strive to provide comprehensive, high-quality care to the communities we serve.
According to the National Alliance on Mental Illness, in 2019, one in five adults in the U.S. experienced mental illness, yet less than half received treatment. Additionally, it is estimated one in six U.S. youth ages 6 to 17 experience a mental health disorder each year, with just 50.6% reporting receiving treatment in 2016.
Even prior to the COVID-19 pandemic, MedStar Telehealth Innovation Center (MTIC) was working with the system’s behavioral health leaders to pilot opportunities for telehealth to support access, efficiency, and more—especially since behavioral health is primarily a cognitive, conversational specialty in which patients may not need to be in-person for physical exams or procedures. The team focused on ambulatory settings and emergency departments (ERs), with inpatient unit pilots as a longer-term goal. Despite initially low patient volumes, lengthy provider credentialing processes, and complex stakeholder needs, promising telehealth models were developed and necessary groundwork laid.
Then, at the onset of the COVID-19 pandemic in March 2020, MedStar Health was faced with an urgent need to sustain behavioral health care, help prevent the spread of COVID-19 among patients and providers, and prepare for a possible surge in the demand for these services based on the new and unique stressors the pandemic was presenting.
Idea
Within weeks of the pandemic reaching the MedStar Health service region, MTIC collaborated with the MedStar Health behavioral health team to quickly implement telehealth solutions. Leveraging a range of platforms, including the Bluestream Health platform used to launch MedStar Health Video Visits in March 2020, the team rapidly developed and scaled telehealth services for multiple behavioral health care settings and needs:
-
Ambulatory individual appointments: Patients can access scheduled, usually one-on-one, appointments via phone and MedStar Health Video Visits.
-
Collaborative care models: Patients can use phone and video to receive care from a team, including a behavioral health care manager, primary care physician, and a psychiatric consultant, who are also using technology to coordinate the care plans.
-
Outpatient group therapy: Beyond in-person group sessions, patients are able to join group therapy via Zoom.
-
TeleCIS and TelePsych in ERs: Patients receiving care in ERs can be seen via video by onsite or remote Crisis Intervention Specialists (CIS) via the Bluestream Health platform during the day, with plans to also include virtual after hours coverage by telepsychiatry provider group partner QLER later in 2021.
-
Inpatient sessions and consults: Providers in the ER, inpatient settings, and working from home, including QLER providers, can consult with inpatients, their families, and other specialists via video.
These platforms have helped us to meet patients where they are and enabled the majority to access care by video outside of a MedStar Health facility—particularly important for those experiencing exacerbated symptoms due to pandemic-related stressors. Additionally, some MedStar Health behavioral health providers have been able to deliver patient care remotely from their own homes and that can also support provider well-being, especially as we all navigate unique challenges during the pandemic.
It is important to note that the public health emergency prompted significant changes to the reimbursement and licensing landscape that made it possible to offer such comprehensive telehealth services in response to the COVID-19 pandemic. It also helped enormously to have related team and partner relationships and pilot programs in place prior to the crisis, which then served as a strong foundation for quickly adapting and responding to COVID-19.
Impact
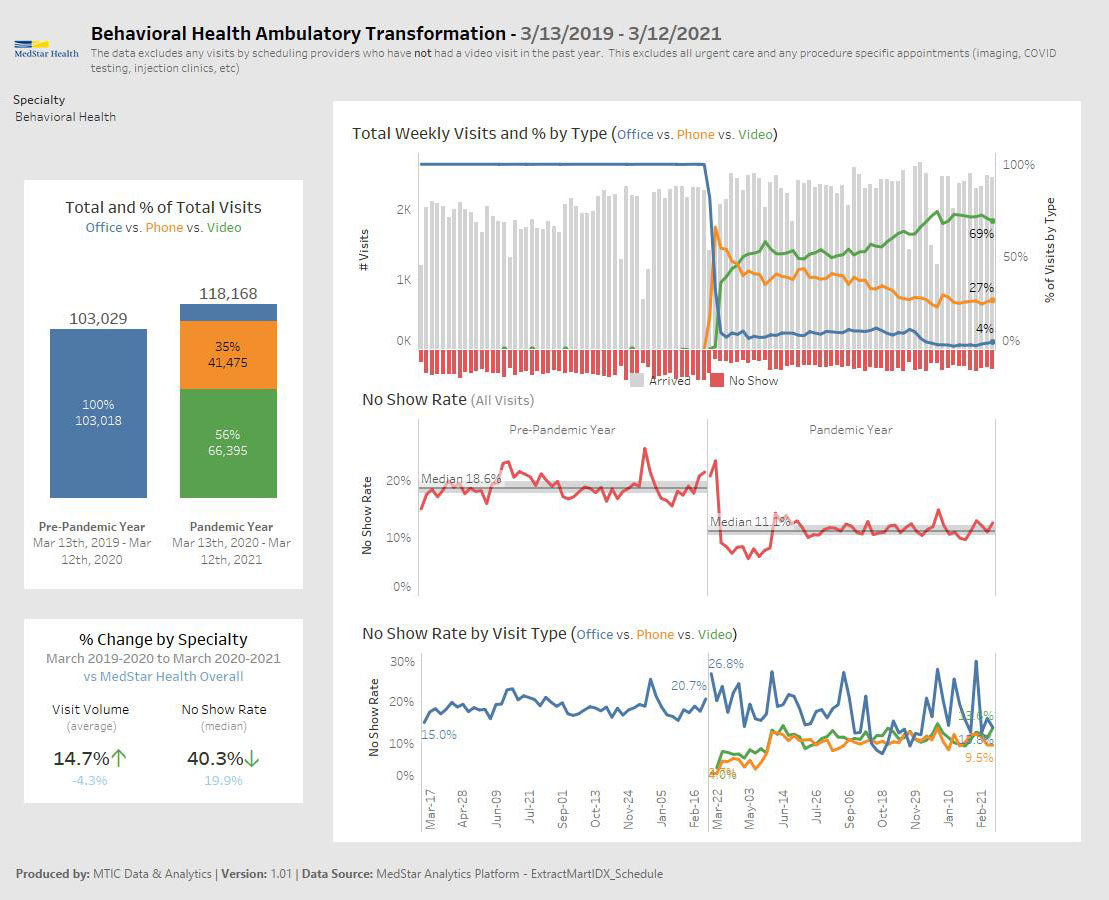
In the year prior to the pandemic, outpatient and emergency department behavioral health telehealth sessions being piloted at MedStar Health were only in the double digits when combined. In the first year of the COVID-19 response, those volumes skyrocketed to an estimated 66,395 scheduled ambulatory video visits and around 4,000 hospital-based video sessions between inpatient encounters, rounding, and ER/CIS interactions.
To provide further context, prior to March 2020, almost 100% of MedStar Health behavioral health care was delivered in-person. At the start of the pandemic, in-office outpatient visits quickly dropped to less than 10% of the overall volume while phone visits increased rapidly. In late March, video visits began to rise with the roll out of MedStar Health Video Visits scheduled outpatient appointments and largely continued to increase throughout the pandemic.
Within a year after the pandemic response launched, telehealth had transformed the behavioral health service line in several notable ways:
-
MedStar Health recovered and exceeded pre-pandemic ambulatory behavioral health volumes in around three weeks, a remarkable pace compared to almost three months to recover primary care volumes.
-
Representing one component of ambulatory volumes, the team started delivering outpatient group therapy by Zoom in late April 2020, holding more than 2,660 sessions reaching 24,660+ participants in the first year of the pandemic response.
-
The ambulatory behavioral health service was still delivering more than 95% of appointments via video and phone as of March 2021, even as other specialties were trending toward primarily in-office visits.
-
In the year prior to the pandemic, there was a median 18.6% patient no-show rate for MedStar Health ambulatory behavioral health appointments. With the rise in phone and video appointments, however, the median no-show rate in the period March 13, 2020 to March 12, 2021 was reduced to 11.1%— a 40%+ reduction in the no show rate year over year. All visit types (in-office, phone, and video) saw a reduction in no-shows thanks to the rise in telehealth usage, helping more patients receive care with existing MedStar Health resources.
As MedStar Health continues to provide behavioral health care during the pandemic, we are also exploring what this telehealth transformation may mean for the future of the service line:
-
With an increase in video visits—and changes to the policy landscape to support growing telehealth needs—comes the possibility of recruiting additional behavioral health specialists from new geographies. This is critical when demand may exceed provider availability in a given area. The partnership we launched with telepsychiatry provider group QLER in 2021 to support the behavioral health service line is an example of the potential.
-
The shift also presents the opportunity to decrease investments in physical office locations and reinvest those resources elsewhere in the service line.
With patients, providers, and leaders increasingly recognizing telehealth’s potential to increase access, efficiency, and patient experience, we hope to see trends noted above extend beyond the pandemic. A key priority of the MTIC team today is informing the future policy landscape to hopefully continue supporting this work, especially based on what we’re learning from the positive reimbursement and licensing frameworks that have been in place during the pandemic. We’re finding reimbursements for both phone and video visits can help reduce barriers to behavioral health care for otherwise vulnerable populations who do not have the same access to, or sometimes preference for, in-office care.
Resources
Websites
News
-
Washington Post, “MedStar Health reaches 500,000 telehealth visits during pandemic”
-
PR Newswire, “Bluestream and 2,300+ Small and Large Health Providers Combat COVID-19 with Free Virtual Care Solution”
-
U.S. News & World Report, “Innovative Telehealth Programs Across Medical Specialties”
Testimonials
“Telehealth has a significant impact on our behavioral health services, especially for outpatients. It has supported an extraordinary drop in the patient no show rate and improved access and convenience. This is especially true for our most vulnerable patients, who otherwise have to take several buses to get to the clinic in addition to arranging for childcare and time off from work. Telehealth also gives us a better appreciation of a patient’s environment, making it easier to engage family members in care or even enabling us to recognize risk at times. On one occasion, our team discovered a possible source of harm in the background of a video session and could intervene and secure it properly. Given these exceptional contributions to patient care, we believe telehealth will remain essential to the future of our service line.”
- Elias K. Shaya, MD, Regional Medical Director and Senior Associate Executive Director for Behavioral Healthcare, MedStar Health
“Telepsychiatry [inpatient video visit] has proved to be an excellent tool and allowed us to run at full capacity and maintain all beds open, having the same patient flux as before the pandemic. With the help of [MedStar Telehealth Innovation Center], we were able to implement a process that allowed one of our providers (who was unable to work on site) to continue to see patients on the inpatient behavioral health unit. We did so with minimal disruptions to the flow of the unit and we were able to utilize a provider remotely, which gave the other providers some well needed time off. The platform was very easy to use, intuitive, and user friendly. It is incredibly flexible, allowing us to use a variety of devices and adapt to each patient’s needs….We were able to successfully pilot the program for 6 weeks (and ongoing) while sharing some of our experiences with other units around the system who are also implementing similar programs.”
- Corneliu Sanda, MD, Chair of Department of Psychiatry, Director of Behavioral Health Service Line, MedStar Franklin Square Medical Center
Page last updated: 6/26/23
Page first published: 6/17/21
Summary
The team has rapidly launched, scaled, and sustained behavioral health telehealth offerings during the COVID-19 pandemic
Team
MedStar Telehealth Innovation Center in partnership with MedStar Health behavioral health leaders and providers
Status
Active