Our commitment to advancing community health
Dear Friends and Neighbors:
Serving our communities is at the heart of what we do, each and every day. At MedStar Health, we use the best of our minds and the best of our hearts to serve our patients across our 10 hospitals, ambulatory and urgent care locations, and through telehealth and home care services. Our commitment to advancing health doesn’t end once a patient leaves our care. Thanks to technological advancements, enhanced access options and new approaches to the care experience, we continue evolving the myriad ways we serve our communities.
Through a comprehensive approach to health and wellness, we strive to enhance health outcomes through better care that emphasizes prevention, builds awareness and fosters independence—especially in underserved communities adversely impacted by disease, health disparities and socioeconomic barriers to optimal health. Community education and partnerships remain critical to achieving this goal.
The 2019 Report to the Community highlights components of our journey to advance health through a population health lens, including an emergency preparedness program that creates a community of first responders, as well as an initiative that helps patients in rural areas secure reliable transportation to their medical appointments. A mobile app for expectant mothers provides valuable education and resources, and perhaps most importantly—peace of mind—between regular appointments. Through several wellness initiatives, including a healthy cooking course and home-based care for chronic illnesses, patients gain the tools and confidence to take control of their own health and wellness.
It is our ongoing privilege to serve the communities in which we live and work. Supporting a stronger, healthier community goes hand in hand with our mission, but more simply—It’s how we treat people.
Sincerely
Kenneth A. Samet, FACHE
President and CEO
Stephen R.T. Evans, MD
Executive Vice President,
Medical Affairs and Chief Medical Officer
Stories of our work in the community
Throughout Maryland and the Washington, D.C., region, MedStar Health works with communities to increase healthcare access and provide education. Our goal is to improve the health and well-being of all residents as we serve our patients, those who care for them, and our communities.
-
Developing a Community of Immediate Responders
In the video above, Susan Kennedy, senior director of Trauma, Burn and Critical Care, MedStar Washington Hospital Center, speaks about the Stop the Bleed program at MedStar Health.
Stop the Bleed campaign
The shirt you’re wearing right now could save someone’s life. Thanks to a new MedStar Health outreach program, you can learn how to leverage that and more.
MedStar Washington Hospital Center has joined the Stop the Bleed campaign, a national program launched in 2015 by the U.S. Department of Homeland Security in response to mass shootings in the United States. The campaign aims to teach community members how to recognize and stop severe bleeding resulting from car accidents, workplace incidents, playground injuries, shootings and larger-scale emergencies like natural disasters.
The goal is to create a “community of immediate responders,” says Erin Hall, medical director of Community Violence Intervention, MedStar Health, adding that no matter how rapid the arrival of professional emergency responders, bystanders will always be first on the scene.
“This course empowers participants and gives them the tools they need to potentially save a life,” she says.
MedStar clinicians provide Stop the Bleed training courses to schools, businesses, community groups, government organizations and other groups. They teach safe blood-loss management techniques, including how to create a tourniquet with everyday items like a shirt or belt.
By educating themselves about emergency first-aid techniques, ordinary people become the first line of treatment and can save lives.
“It’s just as important for people to learn how to stop a stranger’s blood loss as it is to learn CPR,” says Jack Sava, MD, Chief of Trauma, MedStar Washington Hospital Center. He points out that a person who is bleeding can die from blood loss within five minutes, making it critical to stop blood loss quickly.

Source: U.S. Department of Homeland Security
Stop the Bleed course attendees range from Boy Scout troops to Capitol Building security officers to residents of senior housing communities.
“I learned how to be helpful in a high-stress situation,” said Bethany Anderson, a community member who took the course at the Takoma Park Seventh Day Adventist church. She’s studying to be an audiologist, and was interested in taking the class to understand how to pack wounds and apply tourniquets in emergency situations.
“I think if more people knew how to respond in emergency situations, more lives could be saved,” she says.
-
Delivering Access to Foods That Promote Better Health
Pictured above, Stephanie Banks, a MedStar Community Health Advocate picks up fresh produce from Hungry Harvest.
Food is Medicine–Harvest RX
While the benefits of eating healthy are well known, accessing nutritious foods can be challenging.
That is the case for some patients at MedStar Good Samaritan Hospital. The East Baltimore community around the hospital is known as a food opportunity zone—meaning access to fresh produce and supermarkets is limited.
So when Patricia Johnson, a cancer patient at the hospital, was asked by Joyce Johnson, a MedStar Community Health advocate, whether she would be interested in a program that delivers healthy foods to her door, she saw it as an opportunity to eat better.
“With my illness, it’s good for my health to eat fruits and vegetables,” says Johnson, 64. “But it’s not always easy.”
Launched at all three MedStar Health Baltimore hospitals in October 2018, and funded in part by a grant from the PNC Foundation, Food is Medicine–Harvest RX is designed to fill gaps in access to food and nutrition.
MedStar Community Health advocates are trained to identify patients in need of food assistance, enroll them in the program, and give them advice on nutrition and eating healthy on a budget. Then, the patients receive a biweekly box of fresh vegetables, fruits and grain from nonprofit organization Hungry Harvest. The box is estimated to provide four to eight meals.
The program ends after eight weeks, but patients can also be connected with longer-term healthy food programs such as Meals on Wheels, Moveable Feast and the federal Supplemental Nutrition Assistance Program.
“Our goal is to provide patients with a tangible solution to improve their health,” says Ryan Moran, director of Community Health for MedStar Harbor Hospital, MedStar Good Samaritan and MedStar Union Memorial. “Many times, access to healthy food plays an important role in whether or not a patient returns to the hospital.”

Source: Baltimore City Health Department – https://health.baltimorecity.gov/food-access/mapping-food-environment
Moran says that more than 250 patients have participated in the program so far, and the response has been positive and encouraging, for both the participants and the community health advocates who work with them.
“This program has such a positive impact on our patients,” says Joyce Johnson, the MedStar Community Health advocate who enrolled Patricia Johnson in Harvest RX. “I am extremely grateful to be in a position to help those who might otherwise go without fresh food and introduce them to a healthier way of eating.”
-
Helping Expectant Mothers Stay Connected and InformedPictured above, Amanda Linzau, a first-time mom-to-be, used the BabyScripts app for updates throughout her pregnancy.
Partnership with BabyScripts
All expectant mothers gain weight during pregnancy. But Amanda Linzau, a first-time mother-to-be, was concerned she was gaining a bit too much.
So she turned to her app for help.
That app is BabyScripts, a Washington, D.C.,-based mobile software used in partnership by Obstetrics/Gynecology (OB/GYN) practices at MedStar Montgomery Medical Center to help guide patients throughout their pregnancies with information and resources tailored specifically to them.
“Now, every week I can check my app to make sure I’m on track with exactly how much weight gain my doctor recommends,” says Linzau, 22. “This is my first baby, so this app helps me know exactly what to expect in each stage of my pregnancy.”
Expectant mothers using the app receive month-specific information on what’s happening, what to do and what to expect through their pregnancies. This includes upcoming tests and bloodwork, nutrition guides, weight and blood pressure tracking, and information on pregnancy-specific topics, such as gestational diabetes, headaches, hemorrhoids, and spotting.
Patients can even receive alerts and updates from their doctor’s office, including changes in office hours, new staff announcements, and weather-related closures.
Dona Griffin, clinical director, Ambulatory Services at MedStar Montgomery, says that patients are finding BabyScripts more informative and useful than the average pregnancy app.
“Knowing that their own physicians endorse the information provided on the app makes patients feel more comfortable and confident,” she says. “It’s more efficient than going to Google or another app when they have questions. With BabyScripts, they don’t have to think twice about whether their OB agrees with the medical advice they’re receiving.”
Linzau has used other pregnancy apps, and found they only give general information and fun facts. But the customized information she gets with Babyscripts has proven invaluable.

Source: Center for Disease Control and Prevention – https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-complications.html
“I had an appointment coming up for my glucose test, and an alert popped up on my phone telling me what to expect and how to prepare for it,” says Linzau. “That made me feel so much better on the day of my appointment, because I felt like I knew what to expect.”
Indeed, Griffin says MedStar nurses are noticing that patients who use the app come to their appointments more informed, with fewer questions for their doctor. This allows both patients and providers to devote office time to more pressing concerns.
More than 550 MedStar Health patients have used the Babyscripts app. And now, the program has expanded to help mothers even after delivery with one year of postpartum information, resources and updates for mother and baby.
“I’ll definitely use Babyscripts after the baby comes,” says Linzau. “If it helps me during pregnancy, I know it’ll help me after, too.”
-
Helping Seniors Stay in Control of Their Health
Pictured above, Benjamin Jones, Jr., a participant in the TIPS program, gets his blood pressure checked at the Zeta Center.
MedStar Good Samaritan Center for Successful Aging TIPS Program
Every Thursday morning, 75-year-old Benjamin Jones, Jr. learns whether his efforts to keep his blood pressure under control are working.
That’s the day that MedStar Health staff and volunteers visit Jones’s neighborhood senior center, the Zeta Center for Healthy and Active Aging. Jones, along with about 30 other seniors at the center, gets his blood pressure, heart rate, weight and other vital signs checked.
That information is then uploaded to a system that allows a MedStar nurse to review the readings. If any results are of concern or appear abnormal, the nurse contacts the seniors at home to recommend an appointment with their primary care physician for follow up.
“This service helps me determine what I need to do in between my doctor’s visits to keep my blood pressure in the right range,” says Jones, a lifelong resident of the Park Heights area of Baltimore City. “If my blood pressure is high, I know I need to make some changes.”
The weekly service is part of the Telehealth Intervention Program for Seniors (TIPS), a program of the MedStar Good Samaritan Center for Successful Aging. It was created to give low-income adults over the age of 60 a way to stay proactive with their health—and prevent unnecessary emergency department visits and hospital stays.
So far, more than 100 patients at the Zeta Center have enrolled in TIPS.
“We want to reach older adults where they live and engage them in preventative care,” says Carolyn Ford, service line director at MedStar Good Samaritan Hospital, which partnered with the Westchester Public/Private Partnership, the Baltimore City Health Department and the Harry and Jeanette Weinberg Foundation to launch the program in Baltimore. “Being a part of this program shows them how their health can change based on choices they make week to week.”

Source: U.S. Department of Health and Human Services, Administration for Community Living https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OlderAmericansProfile.pdf
When seniors sign up for TIPS, MedStar Community Health advocates also check to see if they qualify for other benefits, such as reduced cab vouchers and Meals on Wheels. These are programs that can also contribute to a patient’s health and well-being, says Ford.
She adds that program participants like Benjamin Jones have found the program helpful, convenient and, most of all, empowering. Jones couldn’t agree more.
“I’m eating better, walking, exercising and cutting back on my salt intake,” he says. “One day I want to get to the point where I’m off my blood pressure medicine entirely. And proud of myself for doing what I need to do to get there.”
-
Improving Access to Care By Providing ‘Wheels to Wellness’
Pictured above is Margaret Hathaway, a patient at MedStar St. Mary’s Medical Center Wheels to Wellness program.
Wheels to Wellness Partnership
“How will I get there?”
For 85-year-old Margaret Hathaway, this was her top concern every time her doctor’s office called to remind her about an upcoming appointment.
Her daughter works full time and can’t always get the day off to take her. Margaret’s ex-husband gives her a ride occasionally, but isn’t readily available. And since she’s not from the area, Margaret has no extended family nearby to help out.
But now she’s got Dave.
Dave is a driver with Wheels to Wellness, a program that helps patients secure reliable transportation to and from medical appointments at MedStar St. Mary’s Hospital.
The program is a partnership between the Tri-County Council for Southern Maryland, The Arc of Southern Maryland, The Center for Life Enrichment and two area hospitals, including MedStar St. Mary’s Hospital.
Wheels to Wellness fills a great need in rural areas of Southern Maryland, where access to public transportation can prove quite difficult.
Bus schedules and availability are sporadic, often causing patients to miss an entire day of work in order to make a scheduled medical appointment. In many cases, patients will simply skip the appointment.
“Consistent and reliable transportation helps patients keep their appointments, which helps keep them healthy,” says Brenda Wolcott, operations specialist, MedStar St. Mary’s Hospital.

Source: National Center for Biotechnology Information – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265215/
Prior to a patient’s appointment, a MedStar associate requests a ride for the patient online through Roundtrip, an online ride scheduling service. The Arc of Southern Maryland or The Center for Life Enrichment fulfills the request and schedules the pickup. Both organizations have vans that would otherwise go unused during most of the workday. The partnership also helps those drivers pick up extra work hours.
In the first 10 months of its partnership with Wheels to Wellness, MedStar provided nearly 1,500 trips for patients.
For patients like Margaret Hathaway, every trip is a “blessing.”
“For those of us who don’t have a lot of help or don’t have the money for cabs, this is just a wonderful service,” she says. “Now I don’t have to fish around to find a ride. I know Dave will be here to get me to my appointments, no matter what.”
-
Using Food As Medicine to Combat Chronic Illness
In the video above, community members and Dr. Theresa Stone, co-founder and medical director of the Fresh & Savory Culinary and Lifestyle Medicine program, discuss benefits of culinary medicine and lifestyle changes to promote better health.
Fresh & Savory Culinary and Lifestyle Medicine Program
Lezetta Moyer grows vegetables and herbs in her garden. She lives an active lifestyle, even at the age of 74. Her mother was a dietician, so she’s always been conscious of what she eats. And yet, she still has hypertension.
“It runs in my family, so it seemed unavoidable,” says the retired U.S. Foreign Service Officer. “But I didn’t like the idea of taking medications for the rest of my life.”
So when her primary care physician, Theresa Stone, MD, at MedStar Health at Lafayette Centre, invited her to participate in a program demonstrating how to keep her blood pressure under control with simple lifestyle changes, she jumped at the opportunity.
Lezetta participates in Fresh & Savory Culinary and Lifestyle Medicine, an innovative program founded in 2017 by Dr. Stone and other physicians at the MedStar Institute for Innovation. Fresh & Savory focuses on a “teaching kitchen” concept, where patients learn culinary and other lifestyle skills that promote better health.
“We saw the need to offer something more than medication and procedures to help control cardiovascular disease, diabetes and high blood pressure,” says Dr. Stone, who adds that the idea of “culinary medicine” intrigues many of her patients.
Participants enroll in the program for eight weeks, and meet weekly at the Sports Performance Center at MedStar Lafayette for 90-minute sessions. The program includes fall and spring cycles, with an average of 15 people per session.

Source: National Institutes of Health – https://www.nih.gov/news-events/nih-research-matters/how-dietary-factors-influence-disease-risk and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265215/
The classes are shared medical appointments, allowing each class to serve as a doctor’s visit with insurance carriers.
Diet, exercise, stress reduction, mindfulness, and sleep are some of the topics covered in the first 20 minutes of class, followed by a cooking session in the teaching kitchen. On “Ask the Doc” night, a MedStar physician joins the group to answer questions and engage in discussion while they all enjoy the prepared meal for the evening.
For Lezetta, Fresh & Savory came into her life just in time.
“One day while I was in my garden, I hurt my knee,” she says, adding that the 15 pounds she lost through the program made her recovery much easier. “To me, that just proves that food really is medicine.”
-
Helping Patients Manage Chronic Illness at Home
Pictured above is Geraldine Hubbard, a patient enrolled in MedStar’s My Health@Home Program
My Health@Home Program
When Geraldine Hubbard was diagnosed with chronic heart failure, her doctor prescribed milrinone, a common medication used to treat the condition. Most patients remain on the drug indefinitely.
But she had a different plan for herself.
“When they told me I would be on that medicine for the rest of my life, I knew I didn’t want that,” says Hubbard, 79, of Washington, D.C., With diligence and a commitment to taking her medication as prescribed, checking her vitals, and making changes to her diet, Hubbard defied the odds—and has been off the medication since July 2018.
She achieved her goals with the help of the MedStar Health Home Care program, My Health@Home.
The program aims to help patients with chronic conditions, such as heart failure, chronic obstructive pulmonary disease (COPD), coronary artery bypass graft, and diabetes, take control of their health—starting in their own homes.
Some patients are referred to My Health@Home by their primary care physicians, but most enter the program after discharge from a hospital, rehabilitation center or nursing home, says Carrie Koenig, vice president of Patient Experience and Communication, MedStar Health Home Care.
“After leaving the hospital, the last thing a patient wants is to have to go back,” she says. “They want to heal at home with their families, and that’s what this program makes possible.”
For the first few weeks of the program, registered nurses and therapists visit patients at their home several times per week, and as patients learn to manage their own condition, visits become less frequent.

During home visits, nurses help patients learn how to track and monitor their symptoms, take medications as ordered, maintain a heart-healthy diet and weight, watch the amount of fluid they consume, and make healthy life choices.
Some patients are given a book to log and track their vital signs, while others receive a remote monitoring device, which transmits the information to the patient’s healthcare team. This gives providers a way to intervene quickly if patient’s vitals reach levels of concern.
“We want to identify negative symptoms before they turn into medical emergencies,” Koenig says. Hubbard calls the program a “godsend.”
“It has made all the difference,” she says. “I attribute so much of where I am today to my nurse’s positive way of thinking and the tools she gave me to succeed.”
-
Supporting Patients with Increased Risk for Cancer
MedStar High-Risk Assessment and Cancer Prevention Clinic
The fear of developing cancer is even greater for those with a family history. Now, with the help of a new MedStar Health program, patients with a predisposition to the deadly disease can get the expert support they need to minimize their risk of developing it—or catch it in its most treatable stages.
Launched in 2017, the MedStar High-Risk Assessment and Cancer Prevention Clinic brings together a team of cancer specialists and genetic counselors to help weigh a patient’s risk for cancer and other inherited diseases, develop a plan of prevention, and take the necessary follow-up measures.
The process begins with a two-hour assessment, reviewing family history, lifestyle, genes and other cancer- causing factors. Following that meeting, a patient may pursue genetic testing—which involves sending a small blood sample to a genetics lab for analysis.
For those patients found to be carriers of a cancer gene mutation, but who have not yet developed the disease, the MedStar team provides the guidance they need to make important decisions to minimize risk.
Anna-Lisa Marcum, a patient who falls into this category, sought the support of the clinic to tailor a prevention plan to reduce her risk of developing cancer.
She’s a mother of two whose own mother and grandmother both died of cancer in their 40s.
“Even though I kind of expected it, it was still hard to hear,” she says of learning that she is a carrier of the BRCA-1 gene mutation, the most common cause of inherited breast and ovarian cancers.

Source: MedStar High Risk Assessment and Cancer Prevention Clinic – https://www.medstarcancer.org/high-risk-assessment-and-cancer-prevention/
Working with a team of experts at the clinic, Marcum decided to undergo prophylactic mastectomy surgery and have her ovaries removed to reduce her risk of developing cancer.
While she chose surgical prevention, others who test positive for a cancer gene mutation may elect to undergo more frequent mammograms, MRIs, colonoscopies, and blood tests to keep an eye on their health.
For these patients, there’s a 50/50 chance that their children also will inherit the gene mutation. We need to keep them abreast of the latest screening and surveillance techniques so that they never develop cancer.
-
Mentoring the Next Generation of Human Factors Experts
Pictured above are Dr. Raj Ratwani, Vice President of Scientific Affairs for MedStar Health Research Institute and director, MedStar Health National Center for Human Factors in Healthcare, and Kylie Gomes, a graduate student at the University of Virginia.
MedStar Health Mentoring Program
Human Factors may not be a well-known field of study, but it plays a crucial role in helping hospitals run efficiently, reduce medical errors and enhance patient care.
Through a MedStar Health mentoring program, a new generation of students receive an opportunity to explore this important and innovative field, and contribute to research that can ensure patients receive the best care possible.
The MedStar Health National Center for Human Factors in Healthcare, part of the MedStar Institute for Innovation, is committed to the scientific study of how humans think, work and interact within the healthcare environment.
To further its mission, the center offers year-round mentoring opportunities for students seeking hands-on experience and education in the field of human factors. Participants range from high school students to PhD candidates.
“The caliber of students who have come to the program has been phenomenal,” says Raj Ratwani, director, MedStar Health National Center for Human Factors in Healthcare, adding that students have come from such prestigious institutions as Georgetown University, Catholic University and American University. “It’s a win-win because we get to benefit from these bright minds and their innovative ideas, and the students are able to work hands-on with researchers.”
Students with backgrounds and interests in psychology, computer science, engineering and various medical concentrations complete three months of rigorous study. They work side-by-side with human factors researchers sharing ideas, conducting research and learning from experts, as well as their peers, on ways to enhance efficiency and accurately in the healthcare environment.
For example, human factors may be applied when designing systems to ensure safe prescribing practices, clear communication among teams, and effective relay of patient information.

Source: MedStar National Center for Human Factors in Healthcare
“I saw this as an opportunity to do meaningful, high-impact work alongside highly skilled researchers,” says Kylie Gomes, a graduate student at the University of Virginia, who is majoring in Engineering Systems Development. “What made this experience so unique is that the students brought perspectives from very different backgrounds, both in training and in life.”
Ratwani says one program participant even had his research published in the industry-leading Journal of the American Medical Association (JAMA).
“The program demonstrates that when we all come together, the best research can happen,” Gomes says.
-
Educating the Community About a Life-Threatening Condition
Pictured above are Jeanne Decosmo, director of Clinical Quality at MedStar Health, and Armando Nahum, a father who lost his son to sepsis. Nahum serves as a patient advisor and spokesman for the Sepsis Collaborative.
MedStar Health Sepsis Collaborative
The lives of many Americans are impacted each year by a serious health condition that causes more deaths than breast cancer, prostate cancer and acquired immunodeficiency syndrome (AIDS) combined. Yet, unless it has touched your family, it is likely you’ve never heard of it.
Sepsis is the body’s extreme response to an infection—which can lead to tissue damage, organ failure and death. More than 1.5 million Americans develop this life-threatening condition each year, and more than 250,000 die from it. It is sometimes inaccurately referred to as blood poisoning or toxic shock, which is why many people are unfamiliar with the term “sepsis” until they or their loved ones are affected by it.
But now, a MedStar Quality and Safety initiative is in place to help educate the community about sepsis— and potentially save lives.
The MedStar Health Sepsis Collaborative was created in 2017 as an awareness campaign aimed at patients, family members and emergency department staff. “The goal is to ensure the greater community is as aware of the signs of sepsis as they are of heart attack or stroke symptoms,” says Jeanne Decosmo, director of Clinical Quality, MedStar Health.
The first stage of outreach efforts included the development of easy-to-understand, patient-friendly brochures, posters and videos created by sepsis survivors, family members of patients lost to sepsis, and the MedStar Patient and Family Advisory Council for Quality and Safety.
“This collaboration between patients, family members and the medical community has been key to the program’s success,” says Decosmo.

Source: MedStar Health – https://www.medstarhealth.org/quality-and-patient-safety/sepsis-prevention-educationn/
Armando Nahum, a father who lost his son to sepsis, serves as a patient advisor and spokesman for the initiative.
“Before it happened to my son, I knew nothing about sepsis,” says Nahum, whose son developed the condition while in a post-surgery rehabilitation facility. “If only I had been more educated, maybe my son would be alive today.”
In addition to educating the public, the initiative also focuses on improving emergency department triage processes for recognizing and treating patients who arrive exhibiting symptoms of sepsis.
“Early identification and treatment are so crucial,” says Decosmo. “Every minute, every hour that goes by untreated, increases the chances of death.”
The Sepsis Collaborative has seen success not only across all 10 MedStar Health hospitals—it has also become a national model for hospital systems across the country. In recognition of its impact, the program received the Sherman Award for Excellence in Patient Engagement in 2018.
2019 Community benefit contribution: $374.1M
Each year, MedStar Health contributes more than $300 million in community benefit services to improve the health of our communities. Community benefit services are programs or activities that provide treatment or promote health and healing as a response to identified community needs. From delivering community health improvement programs to providing care for those who cannot afford to pay, conducting research to advance health and educating the next generation of health professionals, MedStar Health is dedicated to meeting community needs.
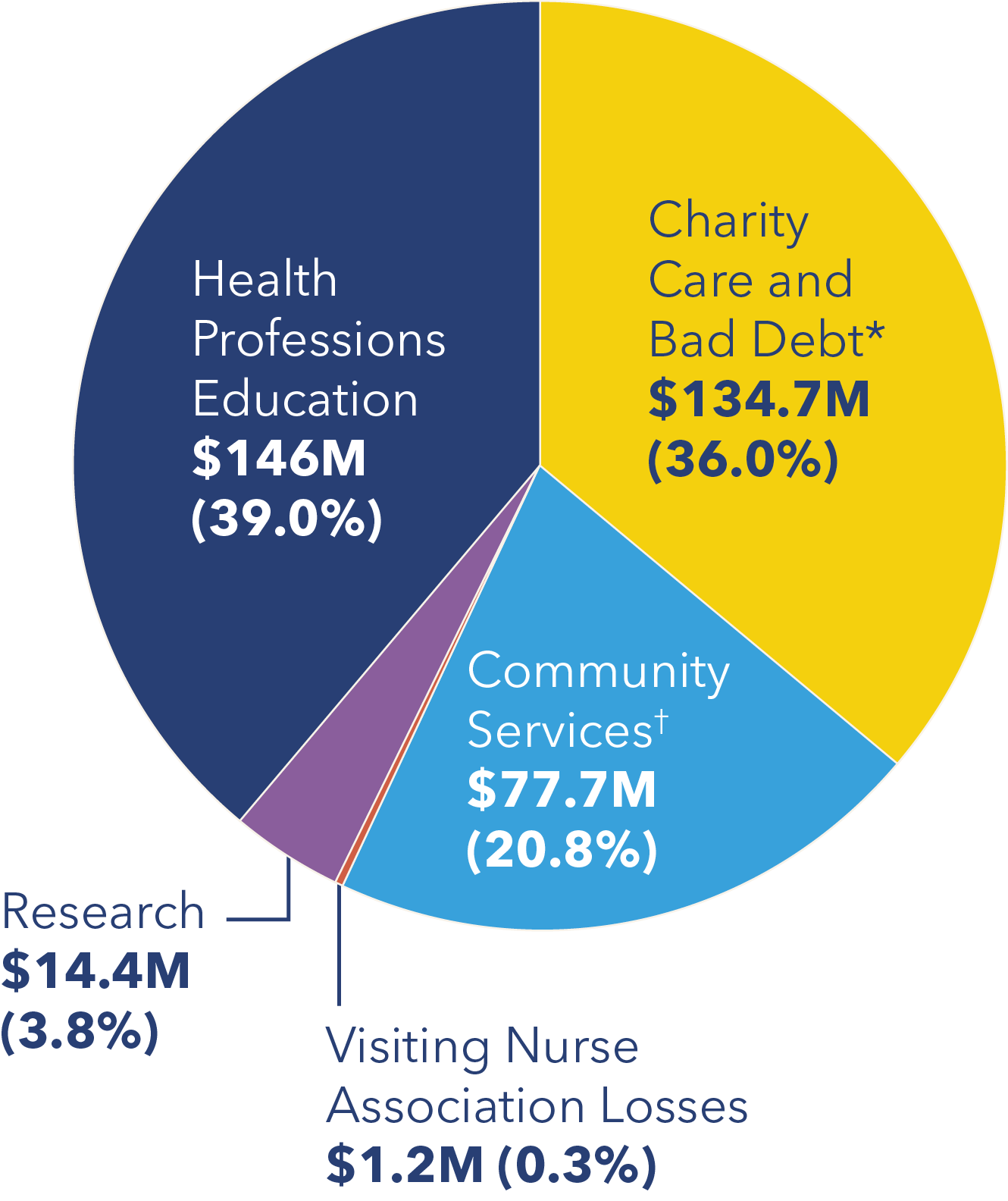
*Includes subsidies, community health improvement services, community building activities, financial contributions, and community benefit operations.
†Includes unfunded government-sponsored programs.
Board of directors
- President and Chief Executive Officer, United Way of the National Capital Area
-
Associate Professor of Neurosurgery and Director of Epilepsy Surgery, Functional Neurosurgery and Pediatric Neurosurgery, MedStar Georgetown University Hospital
-
President, Alabama State University (Retired)
-
Section Chief, Podiatric Surgery, MedStar Franklin Square Medical Center
-
Vice Chairman,
Deloitte (Retired) -
Executive Vice President, Science & Quality, Education and Publications, American College of Cardiology, and Clinical Professor of Medicine at Georgetown University School of Medicine
-
President, MidAtlantic - Bank of America (Retired)
-
Chief of Orthopaedics, MedStar Harbor Hospital
-
President of Ourisman Automotive
-
Chairman, IMC, Inc.
-
President, Georgetown University
-
President and Chief Executive Officer, G.S. Proctor & Associates, Inc.
-
Executive Vice President and Chief Operating Officer, The Bernstein Companies
-
President and Chief Executive Officer, MedStar Health
-
Partner, Brown Advisory, LLC
-
Vice Chairman and Regional Managing Partner, Deloitte (Retired)
-
President and Chief Executive Officer, Danaher Corporation
-
Chief of Cardiology, MedStar Heart & Vascular Institute, MedStar Georgetown University Hospital and MedStar Washington Hospital Center
Corporate executives
-
President and CEO
-
Executive Vice President and Chief Administrative Officer
-
Executive Vice President and Chief Operating Officer
-
Susan Eckert, RN
Senior Vice President and Chief Nursing Officer
-
Executive Vice President, Medical Affairs and Chief Medical Officer
-
Executive Vice President and General Counsel
-
Senior Vice President, Marketing and Strategy
-
Senior Vice President and Chief of Staff
-
Executive Vice President and Chief Financial Officer
-
Eric R. Wagner
Executive Vice President, Insurance and Diversified Operations
-
Senior Vice President and Chief Human Resources Officer
For a list of the entire Leadership Team, visit MedStar Health Leadership.
To learn more about MedStar Health’s programs and initiatives across Maryland and the Washington, D.C., region that are contributing to healthier communities, visit MedStarHealth.org/Community Health or email communityhealth@medstar.net.













