Study data may explain why COVID-19 patients with clinically recognized predisposing factors like obesity, diabetes, liver, kidney and heart disease have more severe disease
WASHINGTON –A study led by the MedStar Georgetown Transplant Institute (MGTI) and published today in the Journal of Hepatology shows that inflammation, resulting from heightened inflammasome activity, leads to immune dysregulation and ultimately severe disease for comorbid patients with COVID-19.
 Early publicized risk profiles related to COVID-19 warned patients with inflammatory comorbidities including: obesity, diabetes, hypertension, and cardiovascular disease were at increased risk of morbidity and mortality due to coronavirus. Included in these populations are patients with liver disease and liver transplant recipients, who are likely to have a co-occurrence of comorbid illnesses.
Early publicized risk profiles related to COVID-19 warned patients with inflammatory comorbidities including: obesity, diabetes, hypertension, and cardiovascular disease were at increased risk of morbidity and mortality due to coronavirus. Included in these populations are patients with liver disease and liver transplant recipients, who are likely to have a co-occurrence of comorbid illnesses.
The study’s lead authors, Dr. Alexander Kroemer, transplant surgeon and MGTI scientific director, Dr. Khalid Khan, medical director of the Islet Cell Transplant Program and Dr. Thomas Fishbein, executive director of MedStar Georgetown Transplant Institute, recognized early on that transplant candidates and recipients were especially vulnerable populations when it came to COVID-19 and decided to better understand how to provide specialized care and treatment.
“Looking into the clinical courses and immune responses of our COVID-19 patients led us to explore the link between immune dysfunction and inflammatory comorbidities,” said, Dr. Kroemer. “Our preliminary data points to that link. The inflammasome and resulting inflammatory cell death, which may contribute to low lymphocyte and T-cell counts, has also been seen in other viral diseases such as HIV.”
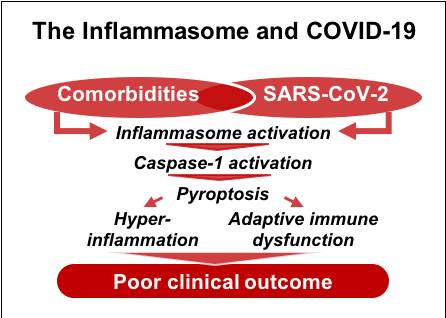
The MGTI study, in collaboration with Amerimmune, a CLIA-certified laboratory, and SUNY Downstate Medical Center, examined the potentially critical role of the inflammasome in COVID-19 patient outcomes. The inflammasome, an intracellular protein complex, monitors and mediates the body’s inflammatory responses to injury or illness. Upon activation, it can induce a form of highly inflammatory cell death called pyroptosis which has two implications. First, it leads to release of pro-inflammatory cytokines, potentially contributing to the so-called cytokine storms that have been reported in severe cases of COVID-19. Second, it can drive immune dysfunction via T-cell and lymphocyte depletion, which prevents the adaptive immune system from mounting an effective antiviral immune response. Viruses such as SARS-CoV-2, which can further activate the inflammasome, could exacerbate and accelerate this detrimental immune response in patients who already have chronic activation.
The study is based on eight COVID-19 liver patients from the MedStar Georgetown Transplant Institute (MGTI), and eight matched COVID-19 non-liver patient controls from SUNY Downstate Medical Center (SUNY). The eight control patients from SUNY were matched based on age, gender, race, comorbidities, and COVID-19 outcome during the same time period.
About MedStar Georgetown University Hospital is a not-for-profit, acute-care teaching and research hospital licensed for 609 beds located in Northwest Washington, D.C. Founded in the Jesuit principle of cura personalis, caring for the whole person, MedStar Georgetown is committed to offering a variety of innovative diagnostic and treatment options within a trusting and compassionate environment. MedStar Georgetown’s centers of excellence include neurosciences, transplant, cancer and gastroenterology. Along with Magnet® nurses, internationally recognized physicians, advanced research and cutting-edge technologies, MedStar Georgetown’s healthcare professionals have a reputation for medical excellence and leadership.
Media Contact
Matthew Holzapfel
571-302-6476 (mobile)
matthew.m.holzapfel@medstar.net









