Severe Asthma Treatment Offers Permanent Solution
(Washington, D.C.,) - Janet Slocum, 70, of Fredericksburg, Virginia enjoys her life-long passion for traveling now without the fear of being hospitalized in an unfamiliar place due to a severe and life-threatening asthma attack.
“I’ve battled serious asthma attacks since I was in my 30s,” says Slocum. “Sometimes I was in the hospital 12 times a year or ended up in an emergency room for my asthma very far from home or missed an important family event.”
Slocum depended on the steroid prednisone in addition to inhalers to keep her asthma under control. Steroids like prednisone prescribed for asthma can cause serious side effects when taken long term.
Then in 2016 Slocum opted for a new treatment called bronchial thermoplasty being offered at MedStar Georgetown University Hospital.
“Bronchial thermoplasty is a series of three bronchoscopies performed about three weeks apart where we heat the airways to destroy or at least weaken the smooth muscles that surround the airways,” says Eric Anderson, MD, director of Interventional Pulmonology at MedStar Georgetown and Slocum’s physician. “People with severe asthma have difficulty with thickening of the smooth muscles around the airways and during an asthma attack these muscles constrict making it hard to breathe. Bronchial thermoplasty is a way of weakening the muscles so the patients don’t have the severity of constriction.”

Bronchial thermoplasty is a painless out-patient procedure performed under general anesthesia and takes about 20-30 minutes. Dr. Anderson inserts a small probe into the airway to send radial current to heat the airways in different places and weaken the smooth muscles around the airways.
“We check breathing tests before and after the procedure to make sure they don’t have an exacerbation of their symptoms due to the procedure,” says Dr. Anderson. “We also give prednisone before and after the procedure to reduce inflammation in the airways.”
Dr. Anderson says bronchial thermoplasty is not a cure for asthma but is a way to eliminate the need for steroids like prednisone, reduce the number of asthma attacks, cut their emergency room visits and improve their quality of life.
Asthma is a disease of the airways that affects 16 million people in the United States and is more common in lower socioeconomic groups. According to the Centers for Disease Control and Prevention, asthma accounts for 1.4 million emergency room visits per year and 10 million doctors’ office visits.
“Unfortunately there are people who still die from this disease,” says Dr. Anderson.
In Washington, D.C., 11-percent of residents have asthma.
After her bronchial thermoplasty Janet Slocum traveled to Australia and New Zealand and remained healthy throughout her trip. Next she ventured to Scotland, Ireland and Wales.
“I’ve gotten rid of a lot of my asthma medications,” says Slocum. “I’ve had no asthma attacks in close to two years.”
“Ms. Slocum was a good candidate for this procedure because due to other health challenges she had to go off of some of the medications that were controlling her asthma,” says Dr. Anderson. “The prednisone was also causing many negative side effects.”
Dr. Anderson says inhalers remain the main treatment for asthma patients after they’ve had the procedure and may be able to come off of oral steroids like prednisone.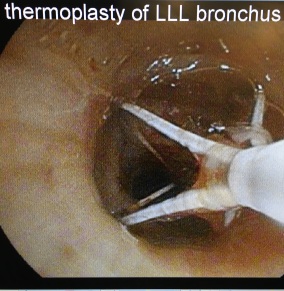
In Washington, D.C., where the incidence of asthma is so high Dr. Anderson believes that more patients should be evaluated for bronchial thermoplasty.
The ideal candidate for bronchial thermoplasty is someone who has severe persistent asthma and asthma flare-ups or someone who depends on steroids or Xolair™ to control symptoms.
Bronchial thermoplasty is not for patients under the age of 18. Patients must be healthy enough to undergo three bronchoscopies and must not be having an acute asthma attack at the time of treatment.
“I’m really doing great,” says Slocum. “In a few months I travel to China and I know I’m going to be truly fine.”
Categories
Media Contact
Marianne Worley
Director of Media Relations
Office: 703-558-1287Pager: 202-405-2824
worleym@gunet.georgetown.edu
Brendan McNamara
Media Relations Specialist
Office: 703-558-1593brendan.t.mcnamara@gunet.georgetown.edu









