Our commitment to advancing community health
Dear Friends and Neighbors:
For more than 20 years, the commitment MedStar Health has had to our communities remains unwavered. The importance of our communities is evident in our longstanding mission to serve our patients and those who care for them. Thanks to new care delivery models, technological advancements, and enhanced access to care, the ways in which we support and serve our communities continue to evolve.
Together with our community partners, trusted providers, and associates, we work to achieve better health through better care, especially across our underserved communities that have been affected by disease, health disparities, and socioeconomic barriers to optimal health. Community education and engagement are critical to delivering this goal and promise.
The 2018 Report to the Community highlights the components of our mission-driven journey to advance health through population health management programs, including a mobile medical clinic that treats children throughout underserved communities, as well as the implementation of a new primary care screening program designed to address the substance abuse epidemic. A safety and wellness program for children helps create and cultivate independence and self-care at a young age, while providing peace of mind for working and single parents. Through chronic disease management programs, patients gain control of their own health and wellness, and a jobs workforce program benefits both patients and health advocates who reside in the neighborhoods they serve.
We are privileged to continue our critical commitment to our communities each year and every day. With your continued partnership, we will advance health and strengthen the communities where we live, work, and serve—for another 20 years.
Sincerely,
Kenneth A. Samet, FACHE
President and CEO
Stephen R.T. Evans, MD
Executive Vice President,
Medical Affairs and Chief Medical Officer
Stories of our work in the community
Throughout Maryland and the Washington, D.C., region, MedStar Health works with communities to increase healthcare access and education. Our goal is to improve the health and well-being of all residents.
-
Building Strength and Independence for Patients With Physical ImpairmentsIn the video above, Dan Evans, a patient of MedStar National Rehabilitation Hospital and Harsh Thakkar, spinal cord injury coordinator, speak about their experiences during the Adaptive Sports and Fitness program.
Adaptive Sports and Fitness Program
Every Tuesday night and Saturday morning, Dan Evans hits the gym. He works with trainers who guide him through resistance training, circuit training, and core strengthening exercises. He chats with fellow gymgoers—the same folks he sees every week—works up a good sweat, then heads home.
But this is no ordinary gym. And Dan isn’t your typical gym client.
He suffered a spinal cord injury in 2007 that resulted in paralysis of his lower extremities. Two years ago, as he was finishing the last of his physical therapy sessions, he knew he needed a way to continue exercising and building his strength.
“I knew that if it were left to me to exercise on my own at home, it wouldn’t get done,” says Dan, a 67-year-old retired attorney for the U.S. Internal Revenue Service. “I was happy to find out that there was a program that could help me continue making progress.”
That program is the Adaptive Sports and Fitness program at MedStar National Rehabilitation Hospital. Its services are completely free, thanks to a grant by the Gordon and Marilyn Macklin Foundation.
The program aims to build and improve strength, muscle endurance, flexibility, functional abilities, and overall mood and confidence for participants with neurological impairments resulting from spinal cord injuries, stroke, multiple sclerosis, and other conditions.
The 4-year-old MedStar Health program was created with the vision to give patients a fitness resource beyond the physical therapy they receive after discharge from a hospital. Most participants come to the program as a referral from their physical therapist, while others find out about the program through our community outreach initiatives and word of mouth.
“The goal is to create a fitness program that resembles what you would find at your local gym,” says Harsh Thakkar, spinal cord injury coordinator, MedStar National Rehabilitation Network. “Except here, we have professionals who are specifically trained to help those with neurological impairments regain their strength.”
Fitness classes include boxing-based fitness, circuit training, and adaptive sports conditioning, among others. Classes can be customized to fit the needs of the individual by certified trainers. Those certified trainers are from DPI Adaptive Fitness, a MedStar Health partner that specializes in dedicated, experienced, and reliable trainers. With backgrounds in physical therapy, personal training, boot camp, boxing, group exercise and adaptive fitness, they set realistic goals for participants and provide services that can safely yet aggressively push people to perform beyond their own expectations.
For those looking for a higher level of activity, the program also offers a wide range of recreational and competitive adaptive sports programs, including wheelchair basketball, quad rugby, cycling, rowing, bocce ball, and others—all open to anyone with a disability at no cost. The sports program provides coaching, training, equipment, and travel assistance, and hosts adaptive sports tournaments throughout the year.
While the physical advantages of these MedStar Health programs are obvious, many participants benefit just as much from the moral support, encouragement, and social enrichment they receive from their peers.
“We’ve seen many people come in for the first time with their heads down, who just want to get their workout done and go home,” Thakkar says. “Then after a while, they are fully engaged and confident with their heads held high.”
That’s certainly true of fitness program participant Dan Evans.
“The strength and endurance I’m building is giving me the ability to stay independent, and that’s vital,” says Evans, adding that thanks to the program, he has the stamina to wheel himself throughout his Dupont Circle neighborhood with ease. “I feel like I can do anything.”
-
Helping Patients With Needs That Extend Beyond Hospital Doors
In the video above, Antoine Langley, community health advocate at MedStar Harbor Hospital and Elizabeth Sebastiao, regional program coordinator, discuss the role of community health advocates in MedStar Health Baltimore hospitals.
Baltimore JOBS Workforce Program
Regina Heath is on her own. The 67-year-old says she doesn’t have the support of family or friends because they’ve all either moved or passed away—making it difficult for her to find someone to drive her back and forth from her many physician appointments.
Her circumstances changed when she was introduced to Antoine Langley.
“He sets up my appointments for me, calls an Uber for me, and lets me know what time they’re going to be here,” says Heath, a resident of Landsdowne and patient at MedStar Harbor Hospital. “Without Antoine, it would be impossible, because I don’t have anybody.”
Antoine is one of over 30 non-medical, entry-level associates who work with high-risk patients from vulnerable communities. The community health advocates and peer recovery coaches are based out of four hospitals—MedStar Franklin Square Medical Center, MedStar Good Samaritan Hospital, MedStar Harbor Hospital, and MedStar Union Memorial Hospital.
The positions are part of the Baltimore Jobs Workforce program and were created to help patients address critical social needs that negatively impact overall health—utility assistance, food, transportation, stable housing, and drug counseling. For example, Antoine’s job might include following up with patients to ensure medication is taken, scheduling transportation to appointments, assisting with registering patients for public benefits, or working one-on-one with patients during routine care following an illness, or managing a chronic condition, such as heart disease.
The program has been a success for patients, participants, and clinicians. The community health advocates live in the neighborhoods they serve, and are therefore able to connect with patients on a more personal level, says Regional Community Health Program Coordinator Elizabeth Sebastiao.
“They can say to the patients, ‘I’ve been in the same spot and I understand’,” Elizabeth says, adding that the program is helping to reduce hospital readmission rates. “Building that relationship of trust makes them feel comfortable opening up and expressing their challenges.”
Since the program began in September 2017, the community health advocates have responded to more than 680 patient encounters, resulting in nearly 4,000 interventions. The peer recovery coaches have worked with more than 280 clients and provided more than 260 referrals to substance abuse resources.

Source: From July 2017 to June 2018 at MedStar Franklin Square Medical Center, MedStar Good Samaritan Hospital, MedStar Harbor Hospital, and MedStar Union Memorial Hospital.
As for the workers themselves, the program has helped them gain confidence about their employment journey and has given them a highly rewarding career path. For community health advocate Antoine, this opportunity couldn’t have come soon enough.
“I had fallen on hard times. I was out of work, and no one wanted to hire me,” says Antoine, a single father caring for three children on his own. So when this second chance presented itself, he jumped at the opportunity to make a difference for himself and his community.
“This is my opportunity to spread knowledge that can help people get over their obstacles,” says Antoine, who went through a four-week training program that included courses on medical terminology, how to document notes, and how to conduct patient home visits. “The most rewarding thing for me is being able to help people in a real way every day.”
-
Helping Children Stay Safe While Home Alone
Pictured above are participants in MedStar Health Home Alone Program
Home Alone Program
Residents in the Olney area have gained a valuable resource to help them with one of the toughest decisions working parents may have to make—leaving a child home alone.
MedStar Health offers the Home Alone program to help prepare 8- to 12-year-olds to spend brief periods of time alone. Participants learn helpful tips about answering the door, keeping the house secure, when to call 911, and other skills.
The program was created five years ago to meet the needs of community members, says Community Outreach Coordinator at MedStar Health, Dairy Marroquin.
“Parents were concerned about that period of time after school—before the parents get home from work,” she says, adding that the program is especially helpful for older children who are left in charge of their younger siblings.
The class is for children only, and is held the third Saturday of every month from 9 a.m. to noon. Taught by certified instructors, the class costs $35 and covers topics such as:
- Understanding the responsibilities of being home alone
- Recognizing emergencies and knowing what to do
- Maintaining a safe environment
- Dealing with strangers on the way home, at the door, and on the phone
- Recognizing when first aid is needed and how to act quickly
- Preparing healthy snacks safely
After the course, children receive a Home Alone handbook that they are encouraged to keep on hand whenever they’re home without adult supervision. The handbook summarizes everything discussed in class, plus important information like emergency phone numbers, first aid tips, and easy microwave recipes.
“I learned the importance of being prepared, calm, and safe when I’m unsupervised,” says a recent class participant. “I use what I learned every time I’m home alone. I don’t open the door for strangers, I’m aware of my surroundings, and I have trusted adults I can turn to.”
Currently, Home Alone classes are only available at MedStar Montgomery Medical Center, but organizers plan to expand the program in the coming year to include other areas of need. Plans include hosting classes at local elementary schools to make the program more accessible for families.
“Through word of mouth, the classes have been very popular,” says Dairy. “Not only are the children leaving the classes more comfortable and confident, their parents are too.”
-
Bringing Expert Medical Advice to Community Members Where They Work and Live
Pictured above, Rajus Chopra, MD, an internist at MedStar Washington Hospital Center, speaks with a community member during an Ask a Healthcare Professional session.
Ask a Healthcare Professional
One Friday afternoon in a meeting room at the U.S. Department of Homeland Security (DHS), about 15 employees came together to discuss cardiovascular disease and high cholesterol.
One person just turned 50, and wondered whether she should start taking a baby aspirin daily to prevent a heart attack, while another wanted to know which heart-healthy foods she should include in her diet.
While these concerns aren’t a matter of national security, they are important questions that internist Rajus Chopra, MD, was more than happy to answer as part of the Ask a Healthcare Professional program at MedStar Washington Hospital Center.
“For participants, this is their chance to connect with a doctor in their own environment,” says Nnenna Oluigbo, MD, MedStar Health internal medicine physician and program coordinator. “They have a lot of questions in these sessions because in their own doctor’s appointments there’s just not enough time to ask everything.”
In addition to workplace locations like DHS, Ask a Healthcare Professional sessions are held at senior wellness centers, community recreational centers, and affordable housing communities in underserved areas throughout Washington, D.C.,
“The goal is to bring resources to the community, and meet them where they are,” says Lindsay Arrington, manager of Community Health Outreach for MedStar Washington Hospital Center.
Topics for Ask a Healthcare Professional include diabetes, cardiovascular disease, hypertension, and breast cancer. Presenters include MedStar Health internal medicine physicians, neurologists, cardiologists, nurses, and diabetes educators.
Sessions begin with a 30- to 45-minute presentation, after which attendees are encouraged to ask any health questions they may have, even if their question does not pertain to the topic of discussion. And while the program was created to benefit the community, participating doctors find it highly rewarding as well.
“The physicians absolutely love it,” Nnenna says. “They feel fulfilled because they can see for themselves that they are making a difference.”
-
Offering College Students Convenient Access to Quality Health Care Right on Campus
Pictured above, Cam Kelley, a junior at St. Mary’s College of Maryland, visits the Wellness Center on campus to receive medical care.
St. Mary’s College of Maryland Partnership
While most college students look forward to a fun and relaxing spring break each school year, Cam Kelley’s breaks were anything but.
“As someone with a chronic illness, I found that all of my breaks were spent running to doctors’ appointments,” says Kelley, a junior at St. Mary’s College of Maryland. “It’s hard to enjoy your spring break when you’re spending most of it at your general practitioner’s office.”
But now, thanks to a partnership between the college and MedStar St. Mary’s Hospital that began in fall 2017, Kelley and all St. Mary’s students have convenient access to expert medical care, right on campus.
When college is in session, a MedStar Health physician’s assistant and medical assistant are on hand for four hours each weekday afternoon at the campus’ new wellness center, making it easy for students like Kelley to get the care they need, when they need it.
“Now, I can work my doctors’ appointments in around my class time,” she says.
Prior to the MedStar Health partnership, students experiencing a medical issue would visit the nurse’s suite only to be referred to a doctor back in their hometown or one outside of school—taking away from valuable class time.

Source: College Health Surveillance Network https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4673518/
“Our campus is located in an area not well served by public transportation,” says Wellness Center Director Laurie Scherer of St. Mary’s College. “Our partnership with MedStar Health gives students more time to attend to their studies, as they may receive great health care right on campus.”
In addition to receiving treatment for everyday student health issues, such as cold, flu, and pink eye, students also have access to expanded women’s health and mental health services, and a medication delivery service that brings prescriptions right to campus. In 2018, 565 students received care at the center.
“St. Mary’s College adds so much to what makes this community special,” says Lori Werrell, director of Population and Community Health. “And we want to do our part to ensure these great students receive the care they need.”
-
Joining Forces to Improve the Well-Being of the City’s Most Vulnerable Children
Pictured above are the medical associates of the KIDS Mobile Medical Clinic/Ronald McDonald Care Mobile in Washington, D.C.,
CVS Health and MedStar Georgetown University Hospital Partnership for KIDS Mobile Medical Clinic
Eleanor Wingfield considers the associates at her doctor’s office more like family. The 55-year-old resident of Southwest Washington, D.C., has been a MedStar Georgetown University Hospital patient for more than 15 years. At first, she would bring her daughter for medical care. Now, her daughter has her own children and they, too, are patients.
However, their doctor’s office isn’t the kind of “office” you might imagine.
Wingfield’s grandchildren are among the more than 800 children seen every year by the KIDS Mobile Medical Clinic/Ronald McDonald Care Mobile®, a 300-square-foot, state-of-the-art MedStar Health medical unit that travels to underserved neighborhoods in Wards 6, 7, and 8, providing medical care to children at no direct cost to their families.
For Wingfield, the mobile clinic gives her family an invaluable medical resource.
“I don’t know what we would do without it. In fact, just yesterday I called because my grandson was really sick,” she says, adding that if she did not have access to the mobile medical clinic, the emergency department would have been the only other option for the toddler, who suffers from asthma. “They got him an appointment the same day, and took excellent care of him, as always.”
And now, thanks to a $150,000 grant from CVS Health, MedStar Health can provide even greater care for children in the area, with expanded services for patients with asthma, mental health concerns, and food insecurity.
The two-year grant has three focus areas: improving the health of children with chronic asthma, addressing food insecurity by helping families access resources to prepare healthy meals, and providing mental health assessments to screen children for Attention Deficit Hyperactivity Disorder (ADHD) and depression. The grant provides the funds for services such as evaluation, social work, and case management.
“This grant enables us to provide an advanced level of care,” says Janine Rethy, MD, chief of Community Pediatrics at MedStar Georgetown University Hospital. “Our goal is to make sure kids reach their potential and thrive in their communities.”
As part of the CVS Health grant, mental health screenings are now fully integrated into routine well-child checkups and new mother visits, with a streamlined system for referring patients to community partners, if needed.
To help asthma patients, the grant funds are used to implement an electronic health records system, making it easier to help patients get the treatment they need.
“With this system, we can look at the big picture and ask ourselves, ‘How can they receive optimal treatment for asthma? Can they afford their medication? Do they know how to use the medication? Can they make it to their follow-up appointments?’” Dr. Rethy says. “Then we can quickly connect them to the resources they need.”
For the third area of focus—food insecurity—the grant is used to implement a screening tool developed by the American Academy of Pediatrics to help identify and assist families who do not have reliable access to food. Children identified as food insecure are referred to community organizations that connect families to food and nutrition resources.
“We can now take our services to a deeper level,” Dr. Rethy says. “This helps us ensure that the children in the communities we serve receive the care they need.”
-
Encouraging Better Health in the Community Through Happy Hour
Pictured above are community members during the Health Happy Hour program at MedStar Southern Maryland Hospital Center
Health Happy Hour
Brenda Brathwaite and a few friends get together once a month for happy hour—where they chat, catch up, and learn about ways to improve their health. Brathwaite is one of the regular attendees of Health Happy Hour, a community wellness program of MedStar Southern Maryland Hospital Center.
About a dozen community residents attend the program on the second Saturday of each month at the District 5 Police Station in Clinton, Maryland. The average age of attendees is between 50 and 75 years old.
Led by certified health, wellness, and fitness professionals, Health Happy Hour topics include identifying heart-healthy foods, reading food labels, reducing stress, cooking healthy over the holidays, and preventing and reversing diabetes.
“I learned how limiting dairy can help with my congestion,” says Brathwaite, 66, who attended the “Boost Your Immune System Now … Food is Medicine” session. “Now I no longer need to take antihistamines on a daily basis.”
Most sessions include an interactive health component. For instance, participants have been introduced to beginner’s yoga and qigong, a method of movement and breathing techniques similar to tai chi.
“I learned about posture, breathing, balance, and techniques for being mindful,” Brathwaite says of the qigong class taught by certified instructor Ann Duvall. “It was great information.”

Source: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion
Participants can choose to have their blood pressure and weight checked during the session, as well as their cholesterol and blood sugar.
“Seeing people become advocates for their own health is so encouraging,” says Rose Dodson, MedStar Health community health nurse. She adds that the overall goal of the program is to help community members achieve and maintain a healthy lifestyle to lower risk of heart disease, stroke, and other serious health conditions. “When participants leave, they share what they’ve learned with family and friends, and that helps make everyone in the community more aware and more informed so they can make healthy choices.”
-
Addressing the Substance Abuse Epidemic Through Primary Care Visits
Pictured above, Anita Tammara, MD, medical director of primary care at MedStar Franklin Square Medical Center, conducts a substance abuse screening with a patient.
Screening, Brief Intervention, and Referral to Treatment at MedStar Franklin Square Medical Center
All patients coming in for a doctor’s visit at the Primary Care Center at MedStar Franklin Square Medical Center are asked the same routine intake questions about their health, medical history, and symptoms—plus a few questions about how often they drink alcohol and use recreational drugs.
Three years ago, questions about alcohol and drug use were not part of routine doctor’s visits. But since the implementation of the Screening, Brief Intervention, and Referral to Treatment program, screening for substance abuse is now the norm for primary care patients. And it’s helping more of them get the help they need.
“Knowing that we ask every patient the same questions regarding drug and alcohol use helps patients feel more comfortable answering openly and honestly,” says Anita Tammara, MD, medical director, Primary Care at MedStar Franklin Square. “And if they screen positive, we can provide the appropriate support and resources.’”
MedStar Health first implemented this program into its Baltimore-area emergency departments as a way to help identify drug and alcohol abuse, address it with the patient, and connect the patient with resources that can help. After seeing the program’s success in emergency departments, it was expanded to Primary Care at MedStar Franklin Square in 2016.
“All 25 resident physicians at the primary care center have been trained in how to address substance abuse concerns in a way that makes the patient feel comfortable and supported,” Dr. Tammara says. With the training, physicians are now more aware of the various treatment resources available to their patients.
Prior to the program, doctors wouldn’t be able to identify substance abuse unless the patient mentioned it or they were demonstrating clear signs of addiction.
“Now that we’re normalizing these discussions between doctor and patient, we’re reducing the stigma,” says Heather Hartman-Hall, MedStar Health behavioral health consultant. “Identifying these issues early helps prevent patients from developing more serious problems down the line.”

Source: Substance Abuse and Mental Health Services Administration, Integration. SAMHSA.gov/Clinical-Practice/SBIRT
Medical Director Dr. Tammara agrees. “The sooner we identify the problem, the sooner we can get patients into treatment, and avoid hospitalization,” she says. “We not only refer them to treatment, we follow up to ensure successful outcomes.”
Since its implementation, the Primary Care Center at MedStar Franklin Square has conducted more than 8,000 screenings through the Screening, Brief Intervention, and Referral to Treatment program.
-
Using Real-Time Technology to Help Patients Control Type 2 Diabetes
Pictured above is Nola Hopkins, a participant in MedStar Health’s Pathway to Diabetes Control Program
Pathway to Diabetes Control
Nola Hopkins was frustrated. As a diabetic, she struggled to keep her A1C level (which measures her average blood sugar level) under control. She ate the right foods, kept herself active, and took her medications on time every day. But still, her A1C remained high.
“Nothing seemed to be working for me and I just didn’t understand why,” says Hopkins, a 58-year-old Fallston resident. “I was about to give up until my doctor told me about this program that could help me.”
That program, offered by MedStar Health, is Pathway to Diabetes Control, a 12-week intensive “boot camp” that gives diabetes patients the education and hands-on support they need to control their diabetes.
To qualify for the program, a patient must have a history of poorly controlled diabetes—usually an A1C of 9.0 or higher. Most patients are referred by their primary care physician.
It didn’t take long after enrolling in the program for Hopkins to get to the root of her problem—she needed to change medications.
“They worked with me to find the right medication and the right dosage to put me on track,” she says. “It was such a blessing to have people right there with me helping me figure this out.”

Source: MedStar Health Diabetes Institute
The program has three steps: self-management education, medication adjustment, and real-time blood sugar monitoring.
On the first visit, participants view educational videos on diabetes management, review and learn more about their current medications, and receive a blood glucose monitor that immediately sends their readings via cellular network to an electronic dashboard. This technology gives MedStar Health diabetes educators real-time monitoring of patient progress.
Participants return after one week to review their readings and adjust medications if needed. After that, the remaining visits are conducted via phone, text or email for an additional eight to 10 weeks.
Michelle Magee, MD, director of the MedStar Health Diabetes Institute, recalls one participant who had had normal blood sugar readings for four weeks, then suddenly recorded a spike. A nurse called him right away to find out what may have contributed to his elevated blood sugar. He told her that he was currently drinking sweet tea at a fast-food restaurant.
“This was a great teachable moment to help that patient see exactly what he was doing, so he could start making proper changes to his behavior,” she says.
The program was developed in 2014 at MedStar Washington Hospital Center, and it has since expanded to eight additional MedStar Health hospitals. More than 600 diabetes patients have participated in the program so far, and the results are remarkable.
“It’s the only program proven to drop A1C by three percent,” Dr. Magee says, adding that program participants have 75 percent fewer hospitalizations within a 90-day period than their peers. “They look and feel so much better after just a few weeks. It’s really rewarding to see patients gain the education and power to take better care of themselves.”
2018 Community benefit contribution: $344.2M
Each year, MedStar Health contributes more than $300 million in community benefit services to improve the health of our communities. Community benefit services are programs or activities that provide treatment or promote health and healing as a response to identified community needs. From delivering community health improvement programs to providing care for those who cannot afford to pay, conducting research to advance health and educating the next generation of health professionals, MedStar Health is dedicated to meeting community needs.
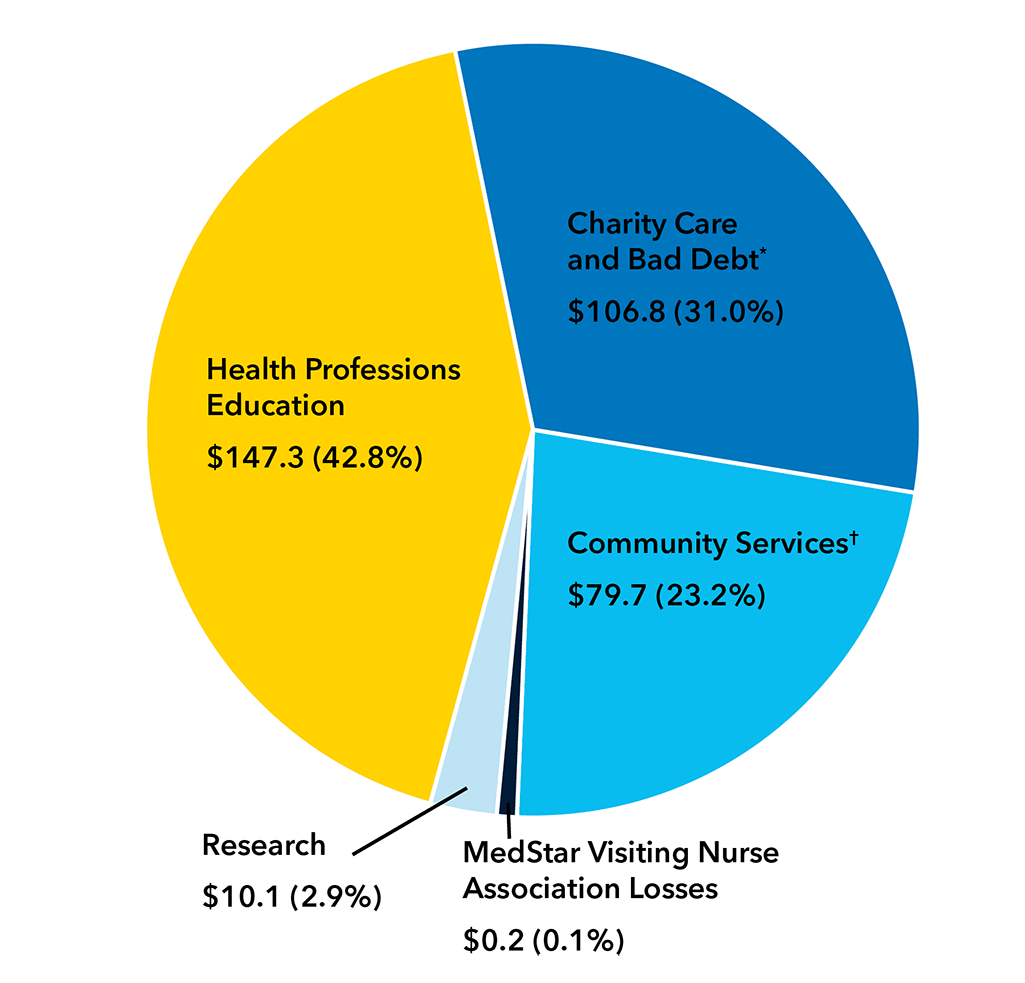
*Includes subsidies, community health improvement services, community building activities, financial contributions, and community benefit operations.
†Includes unfunded government-sponsored programs.
Board of directors
-
President and Chief Executive Officer, United Way of the National Capital Area
-
Section Chief, Podiatric Surgery, MedStar Franklin Square Medical Center
-
Executive Vice President, Science & Quality, Education and Publications, American College of Cardiology, and Clinical Professor of Medicine Georgetown University School of Medicine
-
Vice Chairman,
Deloitte (Retired) -
Retired President, MidAtlantic - Bank of America
-
Chief of Orthopaedics, MedStar Harbor Hospital
-
President, Ourisman Automotive
-
Chairman, IMC, Inc.
-
President and Chief Executive Officer, G.S. Proctor & Associates, Inc.
-
President, Georgetown University
-
President and Chief Executive Officer, WR Roberts Company
-
Executive Vice President and Chief Operating Officer, The Bernstein Companies
-
President and Chief Executive Officer, MedStar Health
-
Partner, Brown Advisory, LLC
-
Co-Founder, Bowie & Jensen, LLC
-
Chief of Cardiology, MedStar Heart & Vascular Institute, MedStar Georgetown University Hospital and MedStar Washington Hospital Center
-
President and Chief Executive Officer, Danaher Corporation
-
Associate Professor of Neurosurgery and Director of Epilepsy Surgery, Functional Neurosurgery and Pediatric Neurosurgery, MedStar Georgetown University Hospital
Corporate executives
-
President and CEO
-
Executive Vice President and Chief Administrative Officer
-
Executive Vice President and Chief Operating Officer
-
Executive Vice President, Medical Affairs and Chief Medical Officer
-
Executive Vice President and General Counsel
-
Senior Vice President, Marketing and Strategy
-
Senior Vice President and Chief Nursing Officer
-
Senior Vice President and Chief of Staff
-
Executive Vice President and Chief Financial Officer
-
Eric R. Wagner
Executive Vice President, Insurance and Diversified Operations
-
Senior Vice President and Chief Human Resources Officer
For a list of the entire Leadership Team, visit MedStar Health Leadership.
To learn more about MedStar Health programs and initiatives across Maryland and the Washington, D.C., region that are contributing to healthier communities, contact Raquel Lamptey at 410-772-6910.

















