Background
Health information systems are rapidly being implemented in a variety of healthcare contexts, including Emergency Departments (EDs). These systems offer promising solutions to challenges related to cost, efficiency, patient safety, and medical errors.
New technologies are often designed with only a limited understanding of the nature of cognition, tasks, and workflow in the setting in which they will be used. Without a careful understanding of how new technologies will be used in practice, unanticipated or undesirable consequences can arise. From increased workload to “workarounds,” patient and provider safety can be compromised if systems and tasks are bypassed, abandoned, or interrupted.
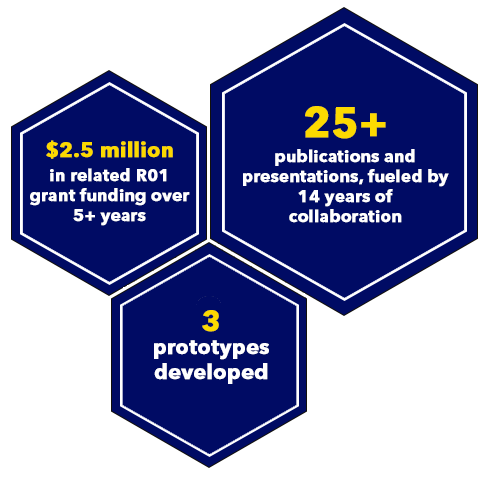
To address these deficits, MedStar Health National Center for Human Factors in Healthcare and MedStar Emergency Physicians recognized an opportunity to leverage their partnership—one of the few existing collaborations between human factors scientists, informaticians, and clinicians. They partnered with the University at Buffalo’s Department of Industrial Engineering to use cognitive systems engineering (CSE) methods to design and test prototype ED information systems. Together, they worked to understand how new technologies will be used in practice, the cognitive work technologies support, and how technologies’ design can be optimized for this support. While there have been applications of cognitive engineering to medical environments, none have provided a comprehensive understanding of the nature of cognitive clinical work and activities across an acute care environment. The research supported by this partnership has continued to grow and has received R01 grant funding since 2014 (R01HS022542; Fairbanks/Hettinger).
Idea
Our goal is to provide a fundamental and comprehensive picture of the difficult sensemaking, decision-making, and planning/replanning tasks in the ED, along with the individual and team expertise required to meet those challenges.
The research uses the ED as a "field laboratory" for two reasons. First, the ED is home to some of the most challenging conditions for cognitive work—high risk, time pressure, and uncertainty—and therefore provides a strong opportunity to generalize findings to other complex healthcare environments. Second, the ED can clearly benefit from the decision aids, visualizations, and other supportive technologies that can result from cognitive engineering analyses.
Additionally, the research will develop and evaluate exemplar solutions for a targeted set of needs that will be identified through the cognitive engineering analysis, thus providing a methodological example and "proof-of-concept" for translating cognitive engineering analyses into designs.
Impact
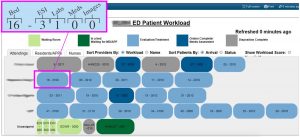
Three main prototypes have been iteratively developed and evaluated leveraging usability methods.
July 2021 Update
Funding for this grant concluded as of September 29, 2020. The research team’s final manuscripts summarizing the last phases of this research are currently under review with peer-reviewed journals. The descriptions provided for the prototypes listed above have been updated to reflect progress since this case study was first written as well. The AHRQ Project Final Report (available here) summarizes the work, publications, and products funded by this research grant in more detail. The health IT vendor community, healthcare organizations, emergency medicine frontline staff, and healthcare researchers can all benefit from these findings.
Acknowledgments
We would like to thank our internal research team, MedStar Health collaborators, and partners from the Department of Industrial Engineering at the University at Buffalo State University of New York, Roth Cognitive Engineering, and Department of Emergency Medicine at the University of Florida for their support, dedication, and teamwork in completing this research in an exemplary fashion.
Key team members include: Aaron (Zach) Hettinger (Principal Investigator), Rollin (Terry) Fairbanks, Ann Bisantz, Emilie Roth, Shawna Perry, Robert Wears, Tracy Kim, Joseph Blumenthal, Sonita Bennett, Shrey Mathur, Xiaomei Wang, Sudeep Hegde, Daniel Hoffman, Natalie Benda, Rebecca Berg, David LaVergne, Lindsey Clarke, Nicolette McGeorge, and Jessica Arora.
Resources
Websites
Publications
Key Publications:
-
Journal of Healthcare Informatics Research, “Communication in the Electronic Age: An Analysis of Face-to-Face Physician-Nurse Communication in the Emergency Department”
-
Journal of Biomedical Informatics, “Cognitive Engineering and Health Informatics: Applications and Intersections”
-
Journal of Applied Ergonomics, “Usability Evaluation of an Emergency Department Information System Prototype Designed Using Cognitive Systems Engineering Techniques”
Additional Publications and Presentations:
-
Annals of Emergency Medicine, “Are you Paying Attention? Related Guidance on how Concepts of Attention may Inform Effective Time Sharing of Tasks in Emergency Medicine [Correspondence Letter]”
-
Journal of the American Medical Informatics Association, “Identifying Visual Search Patterns in Eye Gaze Data: Gaining Insights Into Physician Visual Workflow”
-
International Journal of Industrial Ergonomics, “Studying the Impact of Interoperable Electronic Health Records on Workflow in Ambulatory Care”
-
Journal of Cognitive Engineering and Decision Making, “Assessment of Innovative Emergency Department Information Displays in a Clinical Simulation Center”
-
Theoretical Issues in Ergonomics Science, “Characterizing the Effect of Interoperability on Healthcare Work: A Novel Framework”
-
Cognitive Systems Engineering in Health Care, 1st Edition
-
IEEE International Conference on Healthcare Informatics (ICHI) Abstract, “Assessing the Usability of a Prototype Emergency Medicine Patient-Centered Electronic Health Record Display”
-
IISE Transactions on Occupational Ergonomics and Human Factors in Healthcare System Design, “Applying Human Factors Design for the Clinical Environment: Development and Assessment of an Interface for Visualizing Emergency Medicine Clinician Workload”
-
Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care, “Assessing Interaction Strategies for Health IT: An Entropy Based Approach”
-
Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care, “Development and Description of a Synthetic, High-Fidelity, Emergency Department Patient Dataset for the Evaluation of Healthcare IT Products”
-
Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care, “Supporting the Work of ED Clinicians: Assessment of a Novel Emergency Department Information System in a Clinical Simulation Center”
-
Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care, “Usability Evaluation and Assessment of a Novel Emergency Department IT System Developed Using Cognitive Systems Engineering Approach”
Please note: Images on this page contain fictitious patient data or are otherwise altered for confidentiality.
The overview above reflects work completed while the MedStar Health National Center for Human Factors in Healthcare was part of the MedStar Institute for Innovation. In July 2020, the Human Factors Center transitioned to its new organizational home, MedStar Health Research Institute, and still remains a key collaborator of MI2. Visit the Human Factors Center website for the latest information on its work.
Summary
Cognitive systems engineering methods can be used to design Emergency Department information systems.Team
MedStar Health National Center for Human Factors in HealthcareStatus
ConcludedPage last updated: 7/1/21
Page first published: 10/9/19