Summary
Connected Primary Care (CPC) enhances patient access, provider experience, and practice efficiency through technology, workforce, and workflow innovation.
Team
MedStar Telehealth Innovation Center and MedStar Medical Group
Status
Active
Background
The modern practice of U.S. primary care has common yet critical pain points with patient access and provider experience that invite innovation:
-
Patient access: Since primary care providers (PCPs) keep full schedules serving traditional patient needs, it can be challenging to find additional availability to serve both new patient appointments and time-sensitive care for existing patients. In fact, past studies have shown it can take an average of 18 to 24 days for new patients to schedule appointments with physicians in some of the largest U.S. cities. PCPs also may have limited data and tools to assist their patients in the self-management of their conditions, which could otherwise help patients avoid unnecessary visits.
-
Provider experience: Meanwhile, providers may struggle to find the desired time to spend on their highest complexity patient needs. They face an incredibly high volume of electronic health record (EHR)-related documentation work and other paperwork, billing requirements, patient emails and phone messages, and low complexity follow up that might be more readily performed by another qualified colleague.
Idea
To address these challenges, MedStar Health has piloted and expanded a Connected Primary Care (CPC) model aimed at enhancing patient access, provider experience, and practice efficiency through technology, workforce, and workflow innovation. While this work started before the COVID-19 pandemic, it was accelerated by the exponential expansion of telehealth services in response to the crisis.
The CPC model creates and deploys a central connected care team of virtual practitioners and virtual staff members who currently serve four key functions that help address patient access and provider burnout:
- Same day/next day video appointments: Typically, these visits focus on serving quick-turn, acute needs of existing patients and finding availability for new patients.
- Remote patient monitoring (RPM) for chronic disease management: This proactive care keeps patients connected from their home and is currently focused on high blood pressure.
- Prescription refills: Algorithmic software is used to assist PCPs with the completion of their requested prescription refills in a safe manner that reduces the physician workload to those refills that truly require their attention. Automated prescription refills can also help routine needs to be processed for the pharmacy in an average of four hours.
- Urgent lab/diagnostic result follow up: This quality and safety function ensures important long-loop results (e.g., those following mammograms and colonoscopies) reach patients in a timely manner.
MedStar Health central connected care offerings were initially driven by three connected care teams affiliated with Olney, South Baltimore, and Southern Maryland. They each leveraged existing groups of 20-25 providers from those respective areas, as well as one fully-dedicated nurse practitioner (NP) and medical assistant (MA) who only worked remotely. These three connected care teams supported 14 MedStar Health office-based practices in these geographic areas.
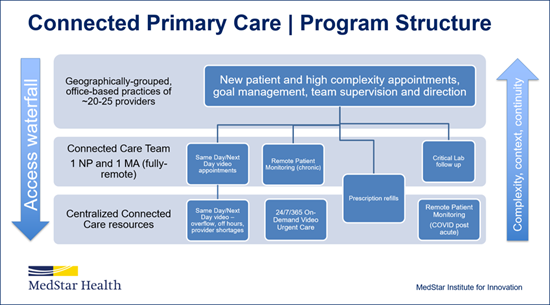 The model also leverages the MedStar eVisit workforce, which traditionally provides on-demand urgent care via telehealth, to offer an additional layer of centralized connected care support as needed. This helps ensure a surge in any of these local primary care contexts can have centralized back up, while keeping teams the right size overall. This team consists of emergency medicine, urgent care, and primary care providers who are acute care specialists: physicians, physician assistants, and nurse practitioners. A day in the life of a centralized connected care provider can be diverse. For example, these providers may start the day with general RPM work and escalations, conduct video visits for their assigned primary care practice, return to RPM work, contribute to MedStar eVisit surge management, and then end their day by resolving RPM escalations. In a single shift, they may serve patients via three different care delivery platforms for three different disciplines—showcasing the flexibility and adaptability of this team.
The model also leverages the MedStar eVisit workforce, which traditionally provides on-demand urgent care via telehealth, to offer an additional layer of centralized connected care support as needed. This helps ensure a surge in any of these local primary care contexts can have centralized back up, while keeping teams the right size overall. This team consists of emergency medicine, urgent care, and primary care providers who are acute care specialists: physicians, physician assistants, and nurse practitioners. A day in the life of a centralized connected care provider can be diverse. For example, these providers may start the day with general RPM work and escalations, conduct video visits for their assigned primary care practice, return to RPM work, contribute to MedStar eVisit surge management, and then end their day by resolving RPM escalations. In a single shift, they may serve patients via three different care delivery platforms for three different disciplines—showcasing the flexibility and adaptability of this team.
Impact
CPC has already experienced rapid growth. During the pilot period, one connected care team supported five office-based practices in the Olney, Maryland area for about six months. This proved the model and prompted greater adoption.
As of Oct. 31, 2021, MedStar Health had delivered more than 2,140 visits via this model after almost a year of activity.
In addition to enhancing patient access, provider experience, and practice efficiency, the CPC model reaches beyond the incremental benefit of adding more people to practices via the dedicated NPs and MAs by including the MedStar eVisit support. The model has proved to be financially sustainable and that makes it possible to scale these services and advance value-based care.
Looking ahead, MedStar Health plans to scale this model to the system’s entire primary care footprint. After about a year of CPC operations, MedStar Medical Group had already posted 12 NP and 12 MA fully-remote job opportunities to support future CPC expansion, also opening the possibility for past MedStar Health associates to rejoin after relocating. Meanwhile, the team is exploring how specialty and hospital care colleagues could potentially help broaden the program’s reach as well.
Scaling Connected Care Models—Fiscal Year 2023 Update
In March 2022, the MedStar Institute for Innovation launched a focus on select priority innovation initiatives and created a community of practice to drive them forward. The Connected Care initiative was established as one of the main focus areas, aiming to widely scale MedStar Health’s successful Connected Care transformation model.
This flexible framework continues to employ telehealth and related technologies, novel workflows, and new remote workforce to deliver improved patient access and experience, associate wellbeing, highest quality and safety care, and financial resilience. In addition to advancing the original functions identified in this model, the team focuses on patient portal message management given the significant increase in the volume of these messages since the COVID-19 pandemic response.
The initiative is on track to achieve system scale in Connected Primary Care in fiscal year 2023 (FY23), and is in the earlier stages of applying the model to care transitions, cardiology, and diabetes.
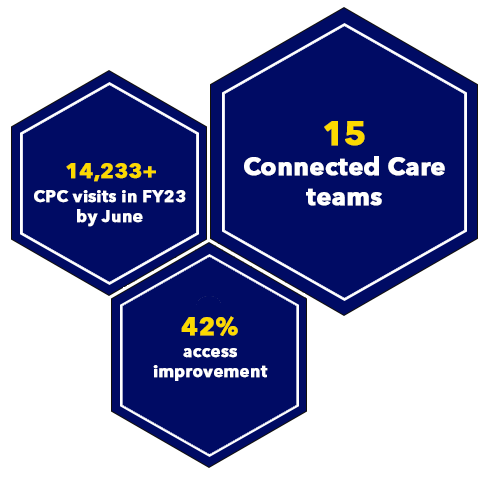
Measuring from our Connected Care scaling efforts starting March 1, 2022 through June 2023, highlights of the results include:
- Adoption: Connected Care nurse practitioners in primary care have delivered 14,233 telehealth visits (FY23 year to date, YTD) and increased productivity of the supported practices. Over 200 patients per month are in active remote monitoring for hypertension management with 52% improvement of control.
- Access: Next available appointment improved 42% for participating providers.
- Experience: The team achieved 24 percentile improvement in the top box Press Ganey patient experience score for supported practices, with an increase in every Press Ganey category (FY23 through 9/30).
- Provider wellbeing: After-hours EHR time decreased 35% for participating providers. Remote teams also handled 218,979 prescription refills (FY23 YTD).
Nearing the end of fiscal year 2023, Connected Primary Care has achieved scale of 15 Connected Care teams that cover the full footprint. The team is also already starting to scale Connected Cardiology given a successful yearlong pilot, in addition to other early successes in applying the model in diabetes care and care transitions.
Resources
Websites
Press Events and Coverage
-
Becker’s Healthcare Podcast, “Ethan Booker, MD, Chief Medical Officer of Telehealth and Medical Director of MedStar Telehealth Innovation Center at MedStar Health” (May 21, 2023)
-
Modern Healthcare, Virtual Health Virtual Briefing, “Opening Keynote: MedStar Health Telehealth: From Crisis Response to Care Innovation” (Oct. 21, 2021)
Testimonial
As a pilot site for the Connected Primary Care (CPC) program, our office has been able to quickly and efficiently provide more rapid-access, on-demand care to our patients. As all primary care clinicians know, it is challenging to provide more same day access while balancing the needs of patients with complex, chronic disease. The CPC program has given my practice and staff the ability to manage patient requests for on-demand appointment access more nimbly. Patients have expressed gratitude that they were able to have a telemedicine visit with our nurse practitioner dedicated to our CPC work on the same day that they contacted our office.
Having a program like CPC also supports primary care clinicians personally. As a physician serving patients in the greater Olney community for more than 16 years and a mother of two young children, it has helped me balance the demands of delivering high-quality, safe, and real-time patient care with the need to make it home in time to care for my family.
- April Tweedt, DO, facility medical director, MedStar Health Primary Care at Olney
Page last updated: 6/26/23
Page first published: 12/14/21