Our commitment to advancing community health
Dear Friends and Neighbors:
On behalf of the MedStar Health family, I invite you to review the 2016 MedStar Health Report to the Community. As the largest not-for-profit healthcare provider in Maryland and the Washington, D.C., region, we are proud of our mission to serve our patients, those who care for them, and our communities. As such, we are dedicated to meeting the diverse and complex healthcare needs of the individuals and families who live and work in the region.
Our vision of advancing health involves a focus on our MedStar Health SPIRIT values. We aim to provide the highest quality care to our patients, pioneer clinical innovation through world-renowned research, train the next generation of healthcare leaders, and work with communities on health and wellness programs. These initiatives focus on the treatment of the whole person, as well as assist our community in increasing access to care and services, addressing social factors such as food access and transportation, and equipping providers with tools to deliver culturally competent and equitable care.
The 2016 MedStar Health Report to the Community highlights examples of the important work we do across our organization to improve community health and benefits in areas like community health services, research and health professions education, as well as community relations and population health. Together, these stories showcase our deep commitment and ongoing investment in realizing optimal health among the individuals, families and communities we are privileged to serve.
Sincerely,
Kenneth A. Samet, FACHE
President and CEO
Stories of our work in the community
Throughout Maryland and the Washington, D.C., region, MedStar Health works with communities to increase healthcare access and education. Our goal is to improve the health and well-being of all residents.
-
 Delivering Food to Those in Need
Delivering Food to Those in NeedMedStar Washington Hospital Center, MedStar Georgetown University Hospital, MedStar Good Samaritan Hospital, MedStar Union Memorial Hospital
The link between nutrition and health is clear. In an attempt to improve patients’ health outcomes, MedStar Health has developed partnerships with food delivery organizations such as Moveable Feast and Food & Friends across the Baltimore and Washington, D.C., region.
Moveable Feast delivers medically tailored meals to people living with chronic and life-threatening illnesses in Maryland, serving more than 5,000 clients each year. They couple their food services—which are delivered right to people’s homes—with medical nutrition therapy services provided by a team of registered dietitians, all at no cost.
“I am so excited about our collaboration with MedStar to help people stay healthy through nutrition,” says Sara Zisow-McClean, director of program services at Moveable Feast. “Together, we have the potential to really impact the quality of life and health outcomes for clients.”
Chronic disease is the primary cause of death and disability in the Maryland / Washington, D.C., region. At least 80 percent of heart disease, stroke and type 2 diabetes and 40 percent of some cancers are preventable through proper nutrition, daily physical activity, and smoking cessation.
Source: World Health Organization, 2011
Food & Friends also sees its relationship with a large health system like MedStar Health as an important and significant way to reach those in need of nutritious meals.
“Our clients aren’t often well enough to prepare food on their own, and many of them also have complex dietary needs due to their health condition,” explains Carrie Stoltzfus, director of program services at Food & Friends. “Malnourished patients have longer and more frequent hospital stays—but so far, 67 percent of our clients report fewer hospitalizations after accessing our program.”
Food & Friends has been serving the Washington, D.C., area for 28 years, providing more than 18 million meals to more than 26,000 individuals. Currently, about 13 percent of their referrals come directly from MedStar hospitals.
Please visit Food & Friends’ and Moveable Feast‘s websites to learn more about the types of services they offer to the community.
-
 Treating the Whole Person: Linking Patients to Social Programs Using Aunt Bertha
Treating the Whole Person: Linking Patients to Social Programs Using Aunt BerthaMedStar Franklin Square Family Health Center, MedStar Harbor Hospital, MedStar Southern Maryland Hospital Center
Erine Gray, founder of Aunt Bertha, Inc., was 17 when his mother developed a life-threatening disease, leading Gray to become her legal guardian after he finished college.
Like many caregivers, it was difficult to find services available for his mother. This inspired Gray to create the Aunt Bertha platform—an online database that makes it easy to identify best-fit programs and trusted, quality services that are nearby to patients.
“Aunt Bertha puts information at the fingertips of clinical providers such as case managers, social workers and patients alike, and brings dignity to the experience of finding help,” says Gray.
In the spring of 2016, MedStar launched the Aunt Bertha pilot project at three outpatient locations: MedStar Franklin Square Family Health Center, MedStar Harbor Hospital Obstetrics Department and the MedStar Southern Maryland Hospital Center Emergency Department. The Aunt Bertha pilot includes two main components: screening patients for unmet social needs as part of the initial intake process and aiding social workers, case managers and medical assistants to link patients with social needs to community social service resources in their ZIP Code.
“Every day, MedStar programs and services [that Aunt Bertha directs patients to] deliver vital care to the most vulnerable in our community,” says MedStar Southern Maryland Hospital Center Emergency Department Director Ryan White.
In addition to expanding access to services, the Aunt Bertha program also presents an opportunity for MedStar to continue identifying and addressing the social determinants affecting patients’ health—taking care of the whole person.
Please visit the Aunt Bertha website to find social services near you.

To date, more than a 1,000 Aunt Bertha searches have been conducted by MedStar providers and staff across the three pilot sites.
-
 Bringing Equity to the Forefront: MedStar Health Research Institute’s Health Equity Plan
Bringing Equity to the Forefront: MedStar Health Research Institute’s Health Equity PlanMedStar Health Research Institute
The Institute of Medicine’s (IOM) 2001 Crossing the Quality Chasm Report points to equity as one of six pivotal aims health systems need to focus on in order to continue to improve the quality of care given to patients. All patients—regardless of race, ethnicity, age, social status, primary language spoken, sexual orientation, level of education, or place of residence—should receive a consistent level of care and have access to the most appropriate resources. MedStar Health Research Institute is committed to health equity and is taking significant steps to extend health equity efforts through the development of its Health Equity Plan.
The Health Equity Plan is a new initiative developed in 2016. It has three goals:
- To ensure equity is a core component of research conducted across the MedStar system.
- To ensure researchers are trained in health equity and research grants are viewed through an equity lens.
- To engage in a participatory and partnered approach to implement the Health Equity Plan.

“We cannot achieve excellence without examining ways to improve the health of our patients, those who care for them and our communities,” says MHRI Health Services Research Executive Director Angela Thomas. “At MHRI, we foster a culture that is sensitive and responsive to the unique needs of diverse patient populations.”
The purpose of the Health Equity Plan is not only to heighten awareness of health equity, but to translate the evidence-based research into improving the patient experience, reducing health care costs and optimizing the health of the diverse populations MedStar serves. Through research, the Research Institute identifies strategies, methods and policies that achieve these goals and move them into practice.
Senior advisors from the Research Institute, in partnership with MedStar administrators, providers, researchers, and academic, clinical, and community partners, are key to advancing the Health Equity Plan and realizing its full impact on patient care.
As Research Institute President Dr. Neil Weissman puts it, “With this initiative, the Medstar Health Research Institute is creating knowledge that leads to a culture of equitable care.”
Please read IOM’s 2001 Crossing the Quality Chasm Report to learn more about IOM’s recommendations for improving health equity in health care systems.
-
Screening for Recovery: Screening, Brief Intervention, Referral to Treatment (SBIRT)
MedStar Franklin Square Medical Center, MedStar Good Samaritan Hospital, MedStar Harbor Hospital, MedStar Union Memorial Hospital
Substance abuse is a public health crisis and has reached epidemic proportions nationally and in the Baltimore region. MedStar Health’s 2015 Community Health Needs Assessment identified addiction as a priority for its four Baltimore hospitals in collaboration with community partners. Data show that patients who have been diagnosed with substance use disorders have more health complications, experience higher costs of care and are readmitted to the hospital more frequently. Implementing the Screening Brief Intervention Referral to Treatment (SBIRT) evidence-based practice is one way MedStar is addressing this epidemic.
SBIRT consists of three main components: screening, brief intervention, and referral to treatment.
Baltimore City Statistics:
- Opioid overdose is a major public health crisis. In 2014, 303 people died of drug and alcohol overdoses, a 19 percent increase from 2013 in Baltimore City.
- Of those who died of overdose in 2014, 192 people died as a result of heroin intoxication. This is more than the number of homicides in Baltimore City that same year.
The SBIRT program is currently offered at MedStar Franklin Square Medical Center, MedStar Good Samaritan Hospital, MedStar Harbor Hospital, and MedStar Union Memorial Hospital. All patients who arrive at the Emergency Departments (ED) at the four hospitals are screened for substance use disorders as part of patient intake through the electronic health record. Patients with positive screens for high-risk behaviors are sent to peer recovery coaches embedded in the EDs to conduct a brief intervention, and to refer to treatment if appropriate.
“Our patients seem more willing to engage in an honest conversation about substance abuse when the discussion is with a peer with lived experience, instead of a healthcare professional who cannot necessarily relate to their lifestyle,” says MedStar Harbor Hospital Emergency Department nurse Cara Miller.
Mosaic Group, a nationally recognized public health consulting firm with expertise in SBIRT implementation in Maryland, partners with MedStar to execute the SBIRT program.
“Having SBIRT allows the Emergency Department to not only take care of the patient’s acute medical issue, but address the underlying substance misuse problem as well,” says Mosaic Group President Marla Oros.
In 2016, MedStar conducted more than 27,000 SBIRT substance use screenings, more than 8,000 brief interventions and made 5,200 referrals to treatment across the four MedStar Baltimore region hospitals.
-
 Providing a Pipeline to Health Care
Providing a Pipeline to Health CareMedStar Health
MedStar Health is committed to building the next generation of healthcare professionals and providing internship opportunities to expose inner-city youth across the region to potential careers in health care. In 1998, MedStar began the Rx for Success program in partnership with the Vivien T. Thomas Medical Arts Academy in Baltimore, located in an area challenged with violence and poverty. The collaboration between MedStar and the school has evolved over the years to create more robust student internship experiences for high-risk youth. Building upon the success of the program in Baltimore, in 2016, MedStar expanded it to Eastern Senior High School in Washington, D.C., through a partnership with Companies for Causes, a nonprofit organization helping at-risk youth graduate and enter college or the workforce.
“The partnership with MedStar provides Eastern Senior High School students extremely valuable opportunities, allowing them to see the connection between their classes and the workplace,” stated Joe Weedon, executive director of Companies for Causes.
Bria Mable is among the participants who were in the program during all four years at the medical arts academy because of its opportunity for professional growth and development. She is now a college freshman studying to be an occupational therapist.

The current healthcare workforce does not accurately reflect our nation’s growing diversity.
When combined, African Americans, Hispanics, and Native Americans represent more than 30 percent of the US population, yet they are significantly under-represented among physicians, registered nurses, dentists, pharmacists, and allied health professionals.
Similarly, Kaheri Gyenyame, a student at Eastern, says that her hands-on internship at the pediatric rehabilitation unit at MedStar National Rehabilitation Network opened her eyes to new future professional opportunities she has in health care.
The Rx for Success program is an eight-week summer internship that connects the course curriculum with tangible onsite experience at one of MedStar’s many clinical sites, and even a few administrative ones, such as healthcare IT. This allows students to demonstrate skill development and experience working in the medical field. New in 2016, interns come together weekly to learn and practice skills in areas such as public speaking, résumé writing, interviewing, and networking. Another newly added component is creating opportunities for community service experiences such as volunteering at Health Care for the Homeless and Shepherd’s Clinic—both MedStar community partners.
Former Executive Director of Shepherd’s Clinic Glenda Skuletich says, “I believe participating in community days like this makes them better health care providers down the road, and that the patients enjoy their role in ‘training’ these students.”
-
 Training Physicians in the Community
Training Physicians in the CommunityMedStar Washington Hospital Center
In addition to providing food pantry services across Washington, D.C., Bread for the City provides primary care services for thousands of underserved, underinsured and uninsured individuals living in the District and has been doing so since 1974. In 2016 alone, Bread for the City saw more than 2,700 patients, totaling more than 12,000 visits
MedStar Health is invested in training future physicians, nurses and other clinical leaders, and equipping them with training opportunities that provide exposure to the diverse needs of the populations they will care for. Each year, 12 resident physicians at MedStar Washington Hospital Center rotate through Bread for the City’s clinic to learn about how social determinants of health play a role in the overall wellness of the patient and impact the care and services patients need. To date, more than 25 resident physicians have participated.
“The Bread for the City clinic provides an opportunity for residents to understand that medical care—though important—is only one of many contributors to the well-being of the patient,” explains Nnenna Oluigbo, MD, internal medicine physician at MedStar Washington Hospital Center. Her residents are among the individuals who participate in the rotations.

The rotation is meant to enhance residents’ clinical skills in an outpatient setting, while teaching them how to identify, understand and address the health needs of low-income individuals and families. The medical residents have a one-month rotation each year at the Bread for the City clinic where they gain invaluable experience in a community-based care setting.
“This training prepares the next generation of physicians to address the public health and social issues that impact their patients’ health, such as housing, education, neighborhood conditions, and socio-economic status,” says Dr. Oluigbo.
-
 Taking a Pledge for Change
Taking a Pledge for ChangeMedStar Health
The Institute of Medicine’s (IOM) 2001 Crossing the Quality Chasm Report points to six areas where healthcare systems need to focus on to improve patient quality. These include providing patient-centered, safe, effective, timely, efficient, and equitable care. Equity is defined as delivering care that does not vary in quality based on a patient’s gender, race, ethnicity, or social and economic status. Such factors often track closely to healthcare disparities. In attempt to eliminate health disparities, the American Hospital Association launched the Equity of Care Initiative in 2015—a call to action asking that hospital and health systems across the United States begin taking action by signing the Equity of Care Pledge.
All MedStar Maryland hospitals signed the pledge in 2016, and multiple efforts are currently underway. The pledge asks hospitals to advance efforts to address health disparities in three domains:
- Governance and leadership diversity
- Patient data stratification by race, ethnicity and language
- Cultural competency training
Specific initiatives at MedStar Montgomery Medical Center include the collection of race, ethnicity and language preference data to support patient-centered culturally sensitive care. For example, a preferred language alert is displayed to all providers when accessing the patient’s health record. The hospital also offers discharge instructions in both Spanish and English, and has added the capabilities to offer Chinese and Russian discharge instructions in the Emergency Department.

The National Center for Cultural Competence provides six reasons health organizations should focus on cultural competency:
- To respond to current and projected demographic changes in the United States.
- To eliminate long-standing disparities in the health status of people of diverse racial, ethnic and cultural backgrounds.
- To improve the quality of services and primary care outcomes.
- To meet legislative, regulatory and accreditation mandates.
- To gain a competitive edge in the marketplace.
- To decrease the likelihood of liability/malpractice claims.
Examples of efforts at MedStar Southern Maryland Hospital Center include increasing the diversity of hospital board members and management in recent years to be more reflective of the community at-large and cultural competency training for employees. MedStar St. Mary’s Hospital collects race and ethnicity preference data to provide culturally competent language line services and cultural competency training as a part of employee orientation.
“I believe in the Equity of Care Pledge and that our purpose is to serve our community by improving health for all and filling in the gaps to meet the community’s needs,” says MedStar Montgomery Medical Center President T.J. Senker.
If you would like to learn more about the Equity of Care Pledge, please visit the American Hospital Association – Equity of Care website.
-
Racing Toward Opportunity
MedStar National Rehabilitation Network
The Super H 5K Run, Walk, and Wheel proves that races aren’t just for running. Started in 2004, Super H 5K participants can run, walk, handcycle, use a recumbent bike, or race in a wheelchair for a great cause.
After a Washington, D.C., area resident Harry Freedman lost his leg in an accident, his friends and family founded the Super H 5K race to raise money for him while he was at MedStar National Rehabilitation Network (MedStar NRN). Since then, Harry’s family and friends have kept the race going to benefit the MedStar Adaptive Sports Program—a program aimed to increase participation in sports among people with physical disabilities.
“The first year, I got Harry in a handcycle so he could participate in the race,” says Joan Joyce, recreation therapy coordinator at MedStar NRN.

The Adaptive Sports Program:
- Provides coaching, training, equipment and travel assistance in nine sports
- Offers circuit training, open gym and cardio fitness classes both at the hospital and in the community
- Hosts adaptive sports tournaments and special events
The Super H 5K has grown over the years and now raises more than $40,000 a year. Race participants include former patients, employees and community residents, with more than 300 participants a year.
“This race is our biggest fundraiser of the year for the Adaptive Sports Program,” attests Tricia Nelson, recreation therapist at MedStar NRN.
Nelson also coaches the MedStar NRN wheelchair rugby team, saying she is dedicated to making the Adaptive Sports Program the greatest of its kind in the country.
“The race is motivational and demonstrates what good health and wellness programs can do to keep those with disabilities functioning at their highest level of performance,” says Vice President of Medical Affairs at MedStar NRN Michael Yochelson. “It allows you to see what someone with a disability can do with the support of rehabilitation services and appropriate equipment. This effort demonstrates our deep commitment to our patients and the community, and continues to be a great way to get our employees engaged in supporting our programs and the individuals they serve.”
Please visit MedStar NRN’s website to register for the next scheduled Super H 5K Run, Walk and Wheel Race.
2016 Community benefit contribution: $340.0M
Each year, MedStar Health invests in the health of the community by providing more than a quarter of a billion dollars in community benefit. Services include teaching the next generation of health professionals, providing care for those who cannot afford to pay, delivering community health programs and services, and conducting research to advance health.

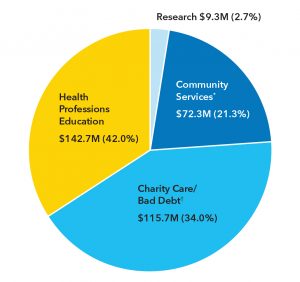
*includes subsidies, community health improvement services, community building activities, financial contributions, and community benefit operations.
†includes unfunded government-sponsored programs.
Board of directors
-
President and Chief Executive Officer, United Way of the National Capital Area
-
Section Chief, Podiatric Surgery, MedStar Franklin Square Medical Center
-
Vice Chairman, Deloitte (Retired)
-
Chairman, TLI Leadership Group
-
Retired President, MedAtlantic - Bank of America
-
President Ourisman Automotive
-
Chairman, IMC, Inc.
-
President, Georgetown University
-
President and Chief Executive Officer, WR Roberts Company
-
Executive Vice President and Chief Operating Officer, The Bernstein Companies
-
President and Chief Executive Officer, MedStar Health
-
Co-Founder, Bowie & Jensen, LLC
-
Chief of Cardiology, MedStar Heart & Vascular Institute, MedStar Georgetown University Hospital and MedStar Washington Hospital Center
-
Associate Professor of Neurosurgery and Director of Epilepsy Surgery, Functional Neurosurgery and Pediatric Neurosurgery, MedStar Georgetown University Hospital
-
Senior Vice President, Capacity Partners
-
Loan Officer, Primary Residential Mortgage, Inc.
-
Executive Vice President of Science,
Education and Quality for American
College of Cardiology and Clinical
Professor of Medicine,
Georgetown University School of
Medicine
Corporate executives
-
President and Chief Executive Officer
-
Executive Vice President
Chief Administrative and Financial Officer -
Executive Vice President and Chief Operating Officer
-
Executive Vice President
Medical Affairs and Chief Medical
Officer -
Executive Vice President and General Counsel
-
Senior Vice President
Marketing and Strategy -
Senior Vice President and Chief Nursing Officer
-
Eric R. Wagner
Executive Vice President, Insurance and Diversified Operations
-
Senior Vice President and Chief Human Resources Officer
For a list of the entire Leadership Team, visit MedStar Health Leadership.
To learn more about MedStar Health programs and initiatives across Maryland and the Washington, D.C., region that are contributing to healthier communities, contact Raquel Lamptey at 410-772-6910.














