Researchers from MedStar Cardiovascular Research Network and MedStar Washington Hospital Center published an international study on a second-generation drug-eluting stent, finding positive and stable outcomes for a bioabsorbable stent in heart patients. “In vivo serial invasive imaging of the second-generation drug-eluting absorbable metal scaffold (Magmaris - DREAMS 2G) in de novo coronary lesions: Insights from the BIOSOLVE-II First-In-Man Trial” was published in the International Journal of Cardiology.
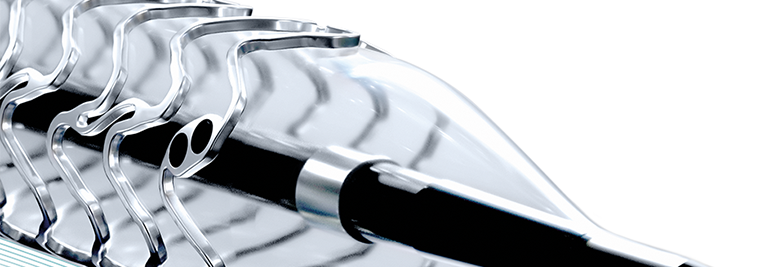
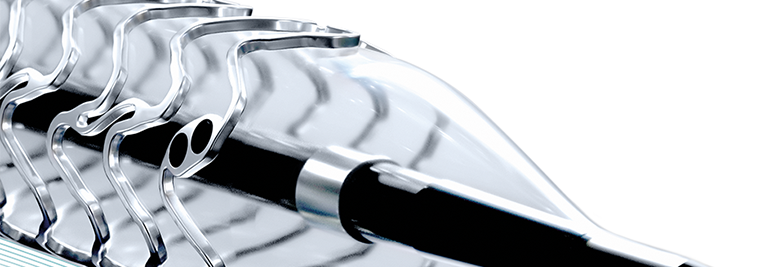
A metallic stent, or scaffold, is a small wire mesh tube that is used to hold open coronary artery to increase blood flow to the heart. Since the development of the first metallic stents in the 1980s, there have been continued improvements in the use of technology for better patient outcomes. Bioresorbable scaffolds are considered a major advancement, designed to decrease the issues found with metallic stents including inflammation and prevention of future surgeries.
The study looked at the imaging results of the 123 participants from eight countries in this first-in-man study. The study evaluated the stent scaffold and the treated coronary vessel through imaging comparisons of baseline, 6-month and 12-month data. The study did find that angiographically assessed coronary vessel curvature was preserved from pre-procedure to the 12 month follow-up period. Imaging included intravascular ultrasound-derived radiofrequency data analysis and echogenicity for evaluation. Through the use of radiofrequency data, the study found dense calcium decreased significantly from post-procedure at 6 months and at 12 months. A build-up of calcium in the heart can lead to a significantly greater risk for heart disease.
“The drug-eluting absorbable metal scaffold DREAMS 2G showed a continuous favorable safety profile and stable performance outcomes up to 12 months,” the study stated. The study concludes that “following the implantation of DREAMS 2G, restoration of the vessel geometry, vasomotion, and bioresorption signs were observed at up to 12 months; importantly, these changes occurred with preservation of the lumen size between 6 and 12 months.”
This research publication was lead by Hector M. Garcia-Garcia, MD, PhD. The research team included Michael Haude, MD; Kayode Kuku, MD; Alexandre Hideo-Kajita; Hüseyin Ince, MD; Alexandre Abizaid, MD; Ralph Tölg, MD; Pedro Alves Lemos, MD; Clemens von Birgelen, MD, PhD, FSCAI, FESC; Evald Høj Christiansen, PhD; William Wijns, MD, PhD; Javier Escaned, MD, PhD; Jouke Dijkstra, PhD; and Ron Waksman, MD. Dr. Garcia-Garcia is the director of angiographic, intravascular ultrasound, optical coherence tomography and near-infrared spectroscopy imaging at the Cardiovascular Core Laboratory, MedStar Cardiovascular Research Network, MedStar Washington Hospital Center (MWHC).
International Journal of Cardiology, 2017. DOI: 10.1016/j.ijcard.2017.12.053