Discover the symptoms of blood clots in the deep venous system and what can cause them
Deep vein thrombosis (DVT) is a blood clot that typically affects the legs and arms. These clots can travel through the bloodstream to the heart, lungs, or brain and cause a stroke or pulmonary embolism.
Our Vein Program specialists will help control your symptoms and reduce the risk of serious complications.
Symptoms
Not everyone will experience symptoms before a clot becomes life-threatening. If you experience any of these symptoms of DVT, see your doctor right away:
- Arm or leg swelling, pain or tenderness
- Warmth in a swollen limb
- Skin discoloration
- Vein dilation
Post-thrombotic syndrome (PTS) is a complication of DVT that causes chronic leg pain, swelling, and discoloration. You may be diagnosed with PTS if blood thinners do not relieve your symptoms. PTS also is called chronic venous insufficiency (CVI).
Causes
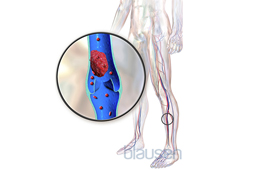
Limited blood flow or having a history of conditions that cause abnormal clotting can increase your risk for DVT.
Some of the risk factors for blood clots include:
- Being obese
- Having a central venous catheter or pacemaker
- Living an inactive lifestyle
- Being pregnant or in the 6-week time period after childbirth
- Being 40 or older
- Taking certain birth control pills
- Suffering trauma to the vein’s inner lining from surgery or injury
Tests
The most common test used to diagnose DVT is the duplex venous ultrasound, which allows your doctor to see the blood flow through your veins. Your doctor may recommend blood tests if your DVT is caused by a genetic condition.
Arterial Duplex Ultrasound for Arms and Legs
Arterial duplex ultrasound uses Doppler and traditional ultrasound to assess blood flow in the arteries of your arms and legs.
Chest X-ray
Chest X-rays use a small dose of radiation to create pictures of the structures inside the chest, including the lungs, heart, and chest wall.
Computerized Tomography (CT) Scan
The cardiac computed tomography scan, or cardiac CT, uses X-rays to create three-dimensional images of your heart and blood vessels.
Fluoroscopy
A fluoroscopy is an imaging technique that uses a continuous X-ray beam passed through the body to create real-time, moving images of your internal structures.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging, better known as cardiac MRI, is a combination of radio waves, magnets, and computer technology to create images of your heart and blood vessels.
Treatments
Your doctor likely will prescribe medications, compression stockings, walking, or lower leg exercises to decrease the risk of blood clots. In some cases, surgery such as venous stenting may be required.
Complex IVC Filter Removal
Complex IVC filter removal procedures are needed when a filter in the inferior vena cava has become embedded in the vessel wall or penetrated the vein.
Rheolytic Thrombectomy
Rheolytic thrombectomy uses a jet of saline delivered through a catheter to break up a blood clot.
Venous Blood Clots Treatments (Venous Thromboembolism)
Venous blood clot treatments may include medications or advanced catheter-based procedures to improve blood flow and reduce the risk of blood clots.
Our providers
Location: Change location Enter your location
-
Emily S. Burman, MSN NP
Hospital Medicine
-
Emma Clelland, FNP MSN
-
Robert Ferris, DO
Internal Medicine
-
Bamlak Andargachew Gebremariam, MD
Hospital Medicine
-
Sumbal Ashraf Janjua, MBBS MD
Advanced Cardiac Imaging & Cardiology
-
Gulzeb Memon, MBBS MD MSPAS
Internal Medicine & Hospital Medicine
-
Vanessa Denyse Olvera, MD
Internal Medicine
-
Shreya Rao, MPAS PA
Cardiology
-
Addisalem Taye Makuria, MD
Hematology and Oncology & Pathology
-
Anteneh A Tesfaye, MD
-
Andrew Chua Tiu, MD
Medical Oncology, Hematology & Internal Medicine
-
Janet C Tsang, MD
Cardiology & Cardiac Electrophysiology
-
Richard Ira Weinstein, MD
Cardiology
-
Amanda Rachel Auerbach, MD
Rheumatology
-
Nabil Badro, MD
General Surgery & Vascular Surgery
-
Gopalakrishnan Srinivasan, MD
Cardiology
Insurance
MedStar Health accepts most major health insurance plans. If you are uncertain as to whether your individual health insurance plan is accepted at MedStar Health, please call your insurance company.









