Featured News
-
February 03, 2026
Philanthropist Genevieve L. Murphy offers a new gift to the J.D. Murphy Jr. Cardio-Oncology fellowship, named for her late husband. COLUMBIA, Md —MedStar Health is pleased to announce the contin...
Browse news by hospital and team
For reporters
Share this
All News
-
 November 19, 2018American Nurses Credentialing Center Magnet Recognition Program® is an Indicator for Excellence in Patient Care
November 19, 2018American Nurses Credentialing Center Magnet Recognition Program® is an Indicator for Excellence in Patient Care -
 November 19, 2018
November 19, 2018In Season of Giving, Family is Thankful for the Gift of Life (Washington, D.C.,) A Virginia father has received a kidney transplant thanks to his son’s organ donation five months earlier a...
-
November 14, 2018
The Breast Center Will Offer Cutting Edge Technologies, Convenient Care BALTIMORE— Bringing together the region’s top breast cancer experts under one roof, MedStar Health Cancer Network opened the Br...
-
November 09, 2018
BALTIMORE — Advancing its enduring tradition of high quality acute inpatient rehabilitation, MedStar Good Samaritan Hospital and the MedStar National Rehabilitation Network in October named Kritis Das...
-
 November 07, 2018
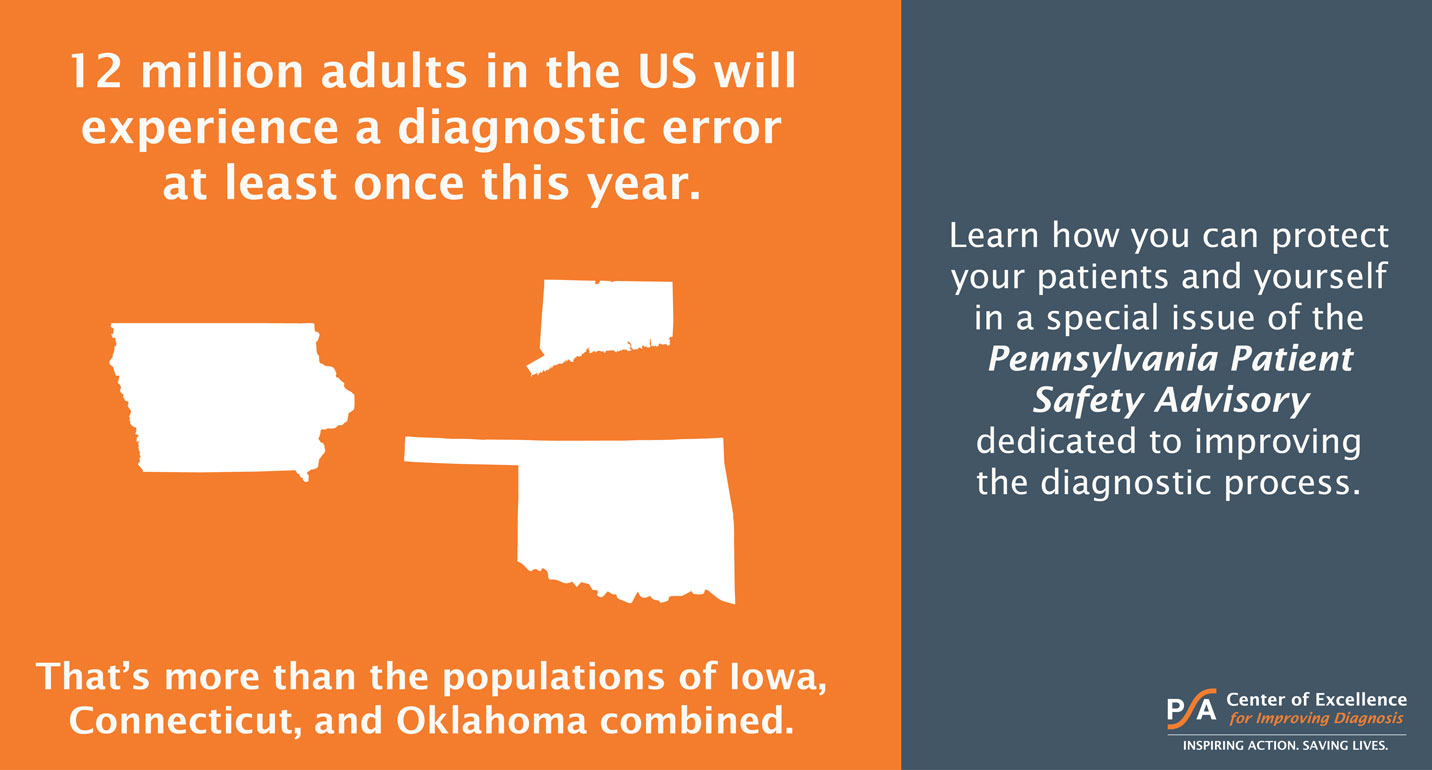
November 07, 2018The Pennsylvania Patient Safety Authority convened a panel of some of the nation's top experts in the field to discuss how to improve the diagnostic process. Featured on the panel was Dr. Christine Go...
-
 November 05, 2018
November 05, 2018Procedure in Minimally Invasive Mitral Valve Repair is First for the Hospital BALTIMORE—A team at MedStar Union Memorial Hospital and the MedStar Heart & Vascular Institute in September successfu...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172














