Featured News
-
November 20, 2025
Nurse-led initiative shows 100% improvement in officers’ ability to identify stroke symptoms. MedStar Health stroke navigators Ariel Woodward, MBA, BSN, and Nicole Goff, MSN, RN, train members o...
Browse news by hospital and team
For reporters
Share this
All News
-
 November 12, 2020
November 12, 2020MedStar Washington Hospital Center First in D.C. and Central Maryland to Adopt HeartFlow Diagnostic Tool Washington D.C., – MedStar Washington Hospital Center became first in Washington, D.C. a...
-
 November 02, 2020
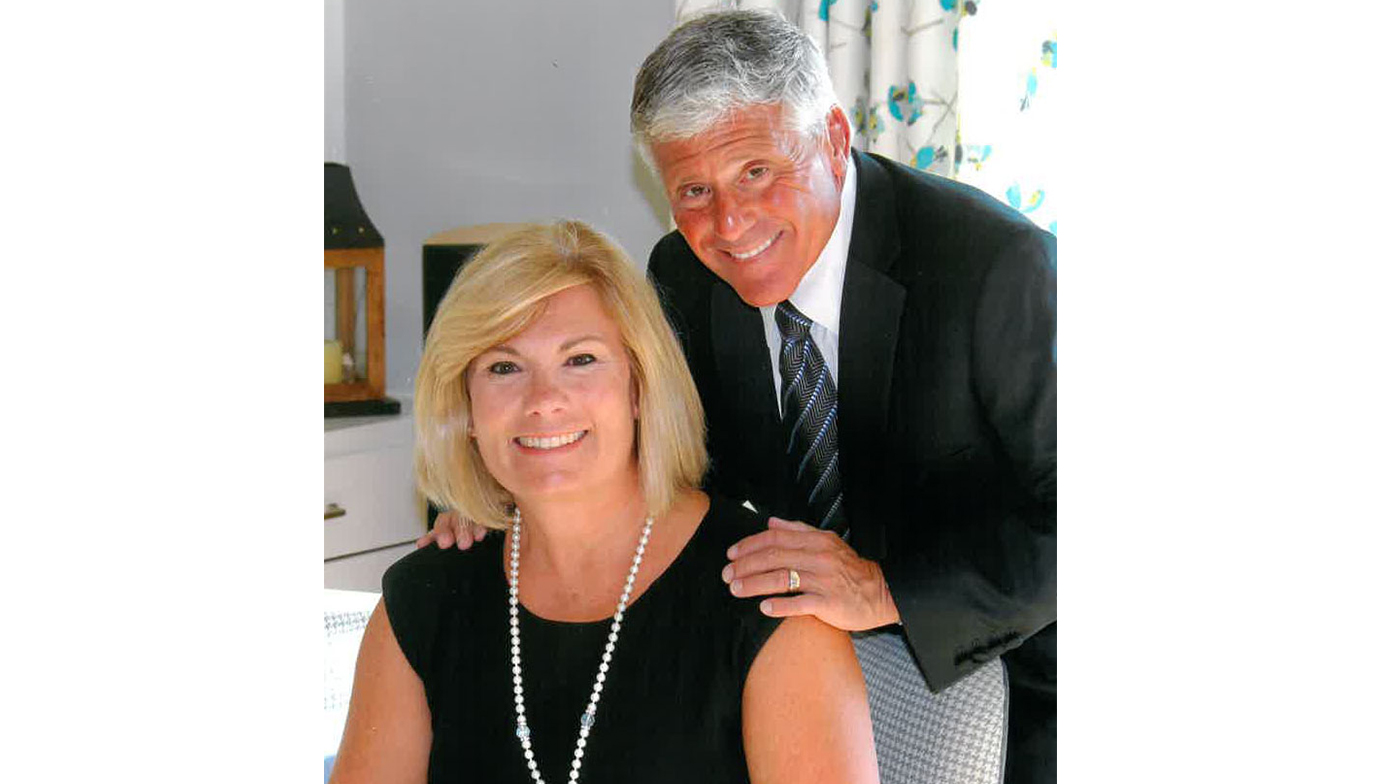
November 02, 2020Washington, D.C., – MedStar Health is honored to announce a generous gift of $4 million from local philanthropists Amy and Alan Meltzer. Mr. Meltzer is CEO and Founder of the NFP | Th...
-
 October 26, 2020As Emergency Departments (EDs) work to best address unique challenges during the COVID-19 pandemic, a study recently published in The Journal of Emergency Medicine by a multidisciplinary MedStar Health team details how integrating telehealth into the ED workflow can reduce healthcare provider infection risk, personal protective equipment (PPE) use, and ED length of stay (LOS), among other benefits.
October 26, 2020As Emergency Departments (EDs) work to best address unique challenges during the COVID-19 pandemic, a study recently published in The Journal of Emergency Medicine by a multidisciplinary MedStar Health team details how integrating telehealth into the ED workflow can reduce healthcare provider infection risk, personal protective equipment (PPE) use, and ED length of stay (LOS), among other benefits. -
October 13, 2020MedStar Washington Hospital Center is First in the U.S. to Use Cirq Technology
-
September 16, 2020
Hyattsville, MD — MedStar Health National Center for Human Factors in Healthcare will be developing computational algorithms and software tools to make the reporting and analysis of patient ...
-
August 11, 2020AHA/ASA Award Recognizes Hospital’s Commitment to Quality Stroke Care
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171















