Featured News
-
December 15, 2025
Partnership will help grow evidence-based programs that studies show reduce sedation rates, improve adherence to treatments, and enhance the overall family experience. COLUMBIA, Md. — MedStar He...
Browse news by hospital and team
For reporters
Share this
All News
-
November 09, 2018
BALTIMORE — Advancing its enduring tradition of high quality acute inpatient rehabilitation, MedStar Good Samaritan Hospital and the MedStar National Rehabilitation Network in October named Kritis Das...
-
 November 07, 2018
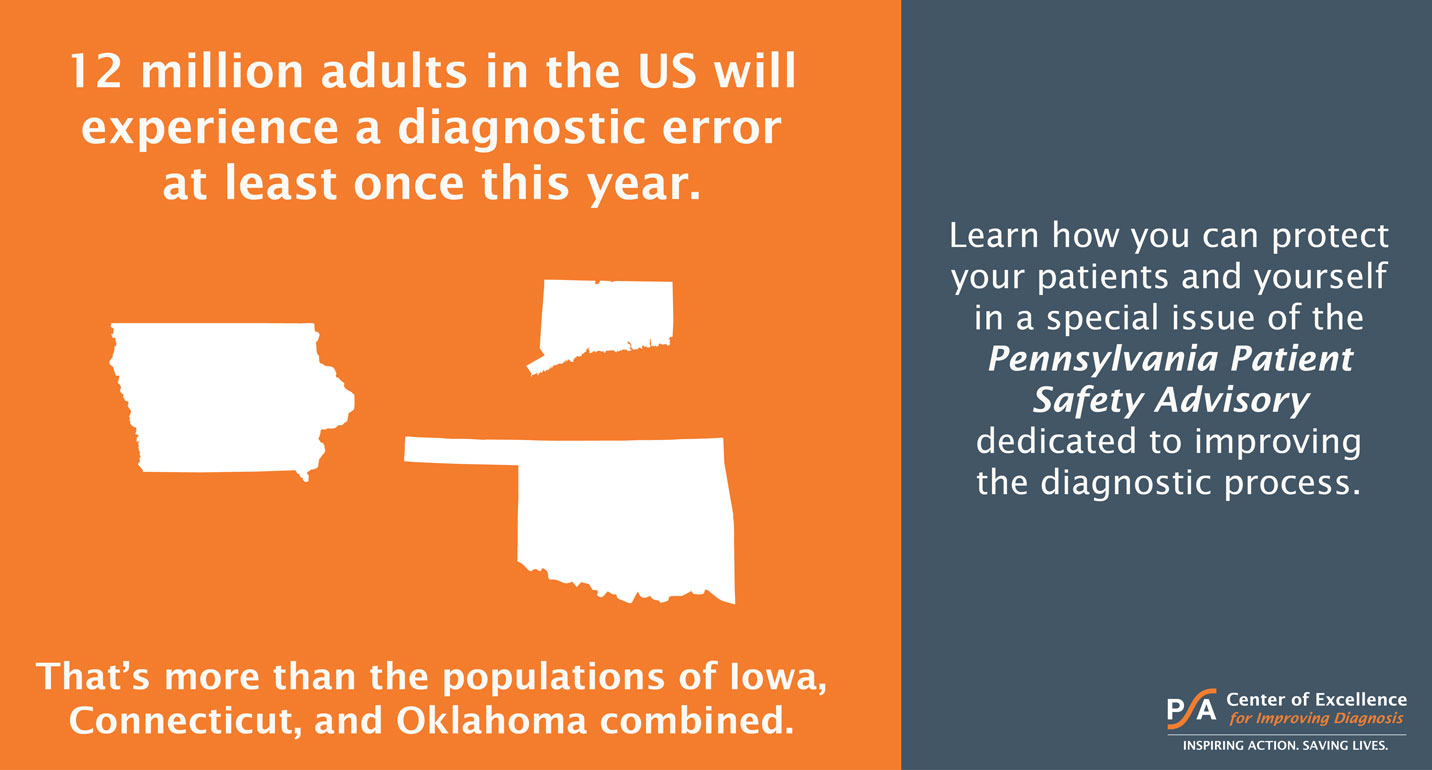
November 07, 2018The Pennsylvania Patient Safety Authority convened a panel of some of the nation's top experts in the field to discuss how to improve the diagnostic process. Featured on the panel was Dr. Christine Go...
-
 November 05, 2018
November 05, 2018Procedure in Minimally Invasive Mitral Valve Repair is First for the Hospital BALTIMORE—A team at MedStar Union Memorial Hospital and the MedStar Heart & Vascular Institute in September successfu...
-
 November 05, 2018
November 05, 2018Makes Procedure More Comfortable, Even Easier to Recover From BALTIMORE—(November 5, 2018)—MedStar Union Memorial Hospital, part of the MedStar Heart & Vascular Institute, has become the first ho...
-
November 05, 2018On Nov. 5, 2018, the health policy journal Health Affairs published an article by MedStar Health’s National Center for Human Factors in Healthcare and its collaborators titled, “Identifying Electronic Health Record Usability and Safety Challenges in Pediatric Settings.”
-
 November 02, 2018
November 02, 2018Patients Can Receive Fresh Produce for Eight Weeks BALTIMORE—(November 2, 2018)—Some MedStar Health patients may be discharged from the hospital with a prescription for healthy food – with a free hom...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171














