Featured News
-
March 06, 2026
MedSTAR Transport teams with the community to support local food pantries. LEONARDTOWN, Md.‒When every second counts, the MedSTAR Transport team is there, on the ground and in the air. They’re t...
Browse news by hospital and team
For reporters
Share this
All News
-
 November 05, 2018
November 05, 2018Makes Procedure More Comfortable, Even Easier to Recover From BALTIMORE—(November 5, 2018)—MedStar Union Memorial Hospital, part of the MedStar Heart & Vascular Institute, has become the first ho...
-
November 05, 2018On Nov. 5, 2018, the health policy journal Health Affairs published an article by MedStar Health’s National Center for Human Factors in Healthcare and its collaborators titled, “Identifying Electronic Health Record Usability and Safety Challenges in Pediatric Settings.”
-
 November 02, 2018
November 02, 2018Patients Can Receive Fresh Produce for Eight Weeks BALTIMORE—(November 2, 2018)—Some MedStar Health patients may be discharged from the hospital with a prescription for healthy food – with a free hom...
-
October 31, 2018
Dr. Kritis Dasgupta Also Named Associate Medical Director, MedStar National Rehabilitation Network BALTIMORE— Advancing its enduring tradition of high quality acute inpatient rehabilitation, MedStar G...
-
 October 29, 2018
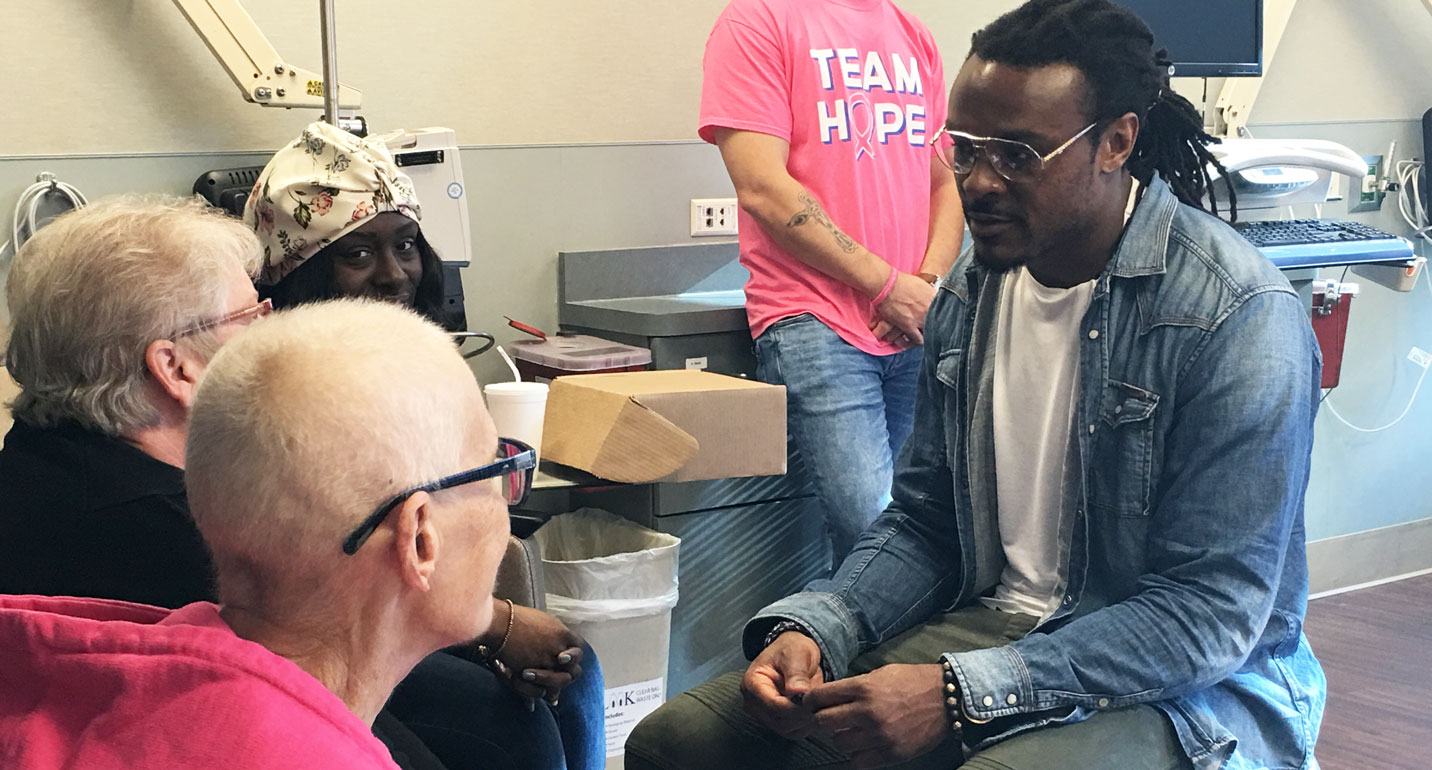
October 29, 2018Cornerback Brandon Carr Distributes HOPE Kits & Wigs Baltimore Ravens cornerback Brandon Carr lifted the spirits of women receiving breast cancer treatment at MedStar Franklin Square Medical Cent...
-
 October 29, 2018
October 29, 2018The Patient Safety Movement Foundation teamed up with the Carter Foundation for the fourth consecutive year in an initiative to eliminate patient deaths and awarded three hospitals based on their comm...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173














