Featured Blog
-
 January 23, 2026
January 23, 2026By MedStar Team
No two individuals’ diets are exactly the same, but we all share one thing in common—we all have to eat! And, most of us enjoy food. In March, the Academy of Nutrition and Dietetics launched their an...
Browse blogs by hospital
Share this
All Blogs
-
 April 05, 2020
April 05, 2020By MedStar Health Research Institute
Researchers from MedStar Washington Hospital Center and MedStar Georgetown University Hospital successfully delivered a healthy baby to a mom and dad who both tested positive for COVID-19. The case re...
-
April 05, 2020
By MedStar Health Research Institute
MedStar Health is participating in a multi-center, randomized, placebo-controlled clinical trial to help evaluate treatment options for patients with COVID-19. We are proud to be contributing to the o...
-
 April 05, 2020
April 05, 2020By MedStar Health Research Institute
Recently published research from a collaborative team from across MedStar Health hospitals sought to compare patient demographics, treatment, and outcomes for Angiotensin-converting enzyme (ACE) inhib...
-
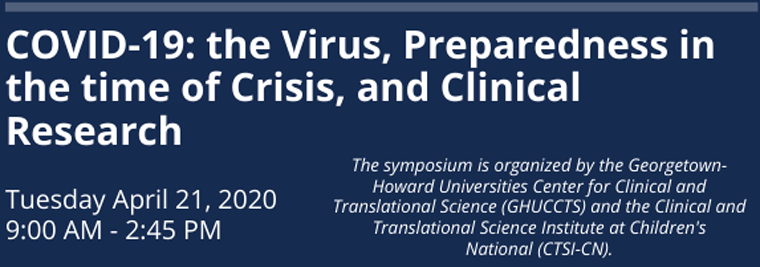 April 05, 2020
April 05, 2020By MedStar Health Research Institute
The Spring Regulatory Update & Hot Topics in Clinical Research conference will be held on Tuesday, April 21 from 9:00am to 2:45pm. This annual meeting brings researchers, administrators, and clini...
-
 April 05, 2020
April 05, 2020Under the Affordable Care Act, large numbers of homeless adults gained Medicaid coverage and policymakers began to identify strategies to improve care and reduce avoidable hospital costs for homeless ...
-
 April 05, 2020
April 05, 2020By MedStar Health Research Institute
Applications are now being accepted for the Pilot Awards for Clinical Translational Studies (PTCS) through GHUCCTS. Applications Submissions are online at PTCS Applications. The completed application...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296














