Featured Blog
-
 February 11, 2026
February 11, 2026Deep inside the liver, billions of protein molecules are produced every day. Sometimes, due to aging or genetic factors a particular protein, transthyretin (also known as prealbumin) can behave badly...
Browse blogs by hospital
Share this
All Blogs
-
 October 31, 2018
October 31, 2018Trick-or-treating is one of the most fun times of the year for kids and parents alike. However, one caveat to the fun can be the masses of sugary treats kids have at their fingertips.With childhood ob...
-
 October 30, 2018
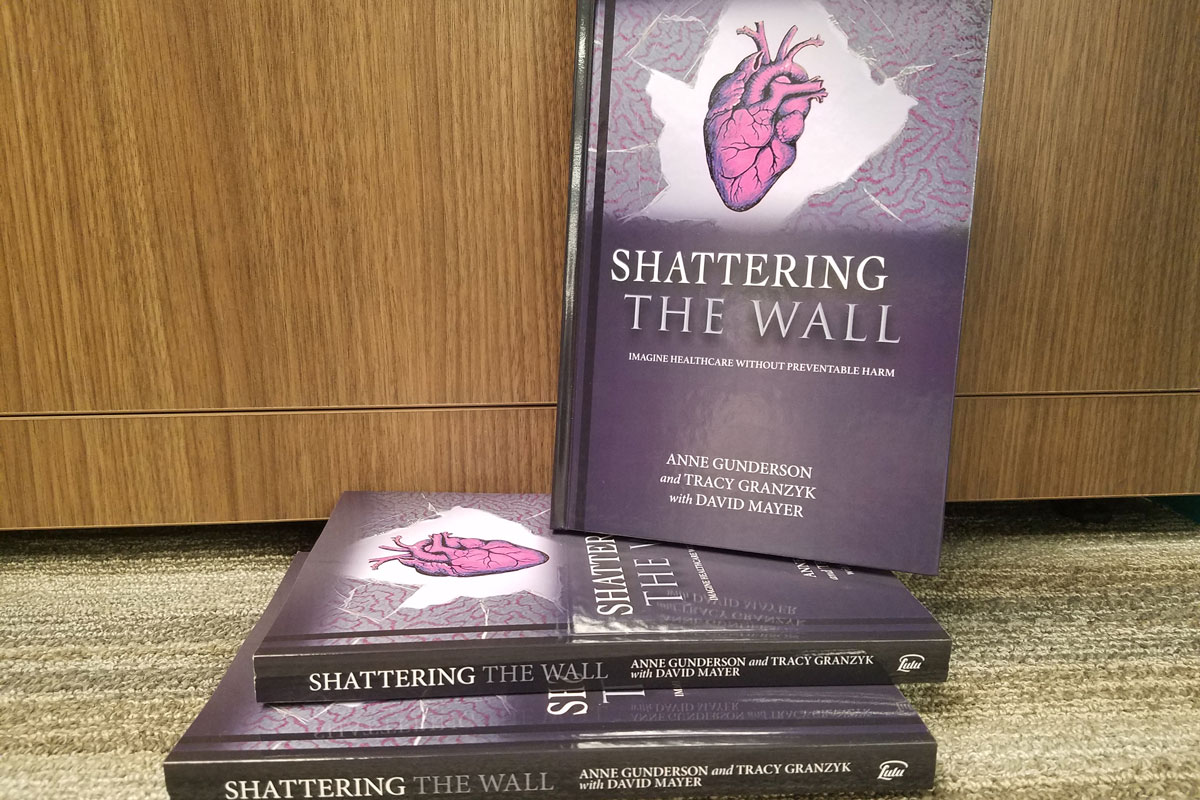
October 30, 2018By Anne Gunderson Ed.D, MS, GNP Since the official creation of The Academy for Emerging Leaders in Patient Safety: The Telluride Experience in 2009, over 800 health science students and residents have...
-
 October 30, 2018
October 30, 2018Surgery is the gold-standard breast cancer treatment, but some techniques leave women flat-chested or with lopsided breasts. Today, many women can benefit from oncoplastic surgery, or oncoplasty, whic...
-
 October 29, 2018
October 29, 2018High blood pressure is a serious problem that continues to grow in our country. Among women of childbearing age, we see about 20 percent with high blood pressure, whether they know it or not. Many pre...
-
October 26, 2018
By Jasmeet Singh Bhogal, MD, MBA
As the weather gets colder, the odds of picking up a respiratory illness like a cold or the flu increase. While both can make you miserable, it’s important to understand the difference, especially if ...
-
October 25, 2018
"Measure twice, cut once.” It’s a simple expression that reminds us to be precise, and it applies in many situations—even complicated neurosurgical procedures.Traditional imaging systems made adhering...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297














