Featured Blog
-
 November 26, 2025
November 26, 2025Since vaccination for smallpox was developed in 1796, the life-saving science of immunization has helped stop the spread of many serious illnesses. Once-common viruses like polio are rare today becau...
Browse blogs by hospital
Share this
All Blogs
-
 May 30, 2018
May 30, 2018By MedStar Health Research Institute
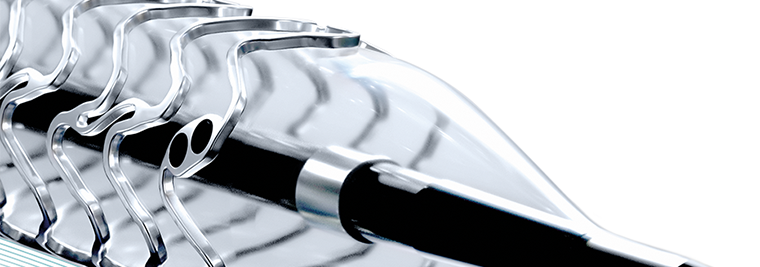
Researchers from MedStar Cardiovascular Research Network and MedStar Washington Hospital Center published an international study on a second-generation drug-eluting stent, finding positive and stable ...
-
 May 30, 2018
May 30, 2018By MedStar Health Research Institute
Congratulations to all MedStar researchers who had articles published in May 2018. The selected articles and link to PubMed provided below represent the body of work completed by MedStar Health invest...
-
 May 29, 2018
May 29, 2018Human papillomavirus (HPV) is the most common sexually transmitted infection in the U.S.—it’s so prevalent that nearly all sexually active men and women will get the virus at some po...
-
 May 29, 2018
May 29, 2018Support for Those With Behavioral Health Needs Two years ago, MedStar Harbor Hospital opened several brand new behavioral health treatment areas devoted to the diagnosis and treatment of conditions r...
-
 May 29, 2018
May 29, 2018Task Force Unites Community to Break Down Barriers MedStar Harbor Hospital is fully committed to meeting the healthcare needs of its community. But knowing exactly what those needs are, and putting t...
-
 May 29, 2018
May 29, 2018 Did you know that Maryland ranks among the states with the highest number of confirmed cases of Lyme disease? The most common infectious disease spread by the bite of ticks, Lyme disease ...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294














