Featured Blog
-
 February 11, 2026
February 11, 2026Deep inside the liver, billions of protein molecules are produced every day. Sometimes, due to aging or genetic factors a particular protein, transthyretin (also known as prealbumin) can behave badly...
Browse blogs by hospital
Share this
All Blogs
-
 May 30, 2018
May 30, 2018By MedStar Health Research Institute
A MedStar research study has found that in 15- to 44-year-old women who receive Medicaid, both implantable long-acting reversible contraceptives and intrauterine devices had high continuation rates an...
-
 May 30, 2018
May 30, 2018By MedStar Health Research Institute
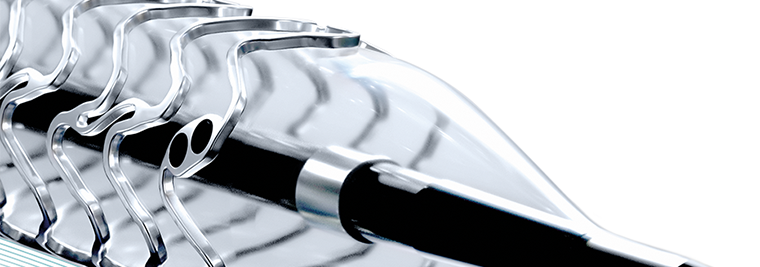
Researchers from MedStar Cardiovascular Research Network and MedStar Washington Hospital Center published an international study on a second-generation drug-eluting stent, finding positive and stable ...
-
 May 30, 2018
May 30, 2018By MedStar Health Research Institute
Congratulations to all MedStar researchers who had articles published in May 2018. The selected articles and link to PubMed provided below represent the body of work completed by MedStar Health invest...
-
 May 29, 2018
May 29, 2018Task Force Unites Community to Break Down Barriers MedStar Harbor Hospital is fully committed to meeting the healthcare needs of its community. But knowing exactly what those needs are, and putting t...
-
 May 29, 2018
May 29, 2018Dedicated Nurse Leader Retires After 45 Years It was more than 45 years ago when Lenora Addison, RN, BSN, MA, first stepped foot into South Baltimore General Hospital— now MedStar Harbor Hospital—to b...
-
 May 29, 2018
May 29, 2018Support for Those With Behavioral Health Needs Two years ago, MedStar Harbor Hospital opened several brand new behavioral health treatment areas devoted to the diagnosis and treatment of conditions r...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297














