Featured Blog
-
 March 06, 2026
March 06, 2026The liver is your largest internal organ, and it performs a range of vital functions, including: Filtering and cleaning your blood of waste products and toxins. Creating bile, ...
Browse blogs by hospital
Share this
All Blogs
-
 March 30, 2020
March 30, 2020Taking cues from how other countries are managing COVID-19, government and healthcare leaders have implemented dramatic and necessary steps to slow its spread. Because there is not yet a cure for thi...
-
 March 26, 2020
March 26, 2020By Elspeth Cameron Ritchie, MD
When an unfamiliar disease strikes, it can cause tremendous fear and anxiety. We’ve seen it before—during the 1918 Spanish flu epidemic and, in more recent times, with HIV, SARS and the a...
-
 March 26, 2020
March 26, 2020Just as flu season comes to an end in the United States, the Novel Coronavirus Disease of 2019 (COVID-19) shows up to thwart your spring break plans. While there are many similarities between t...
-
March 24, 2020
Most people don't like discussing issues with their bowel movements (BMs) or even thinking about them. But the condition of your fecal matter can reveal a lot about your colorectal and overall health—...
-
 March 19, 2020
March 19, 2020Whether playing indoors at the gym or outdoors on the asphalt, basketball-minded weekend warriors must be sure to take proper care of their feet and ankles. What Are the Top Three Basketball Foot and ...
-
 March 17, 2020
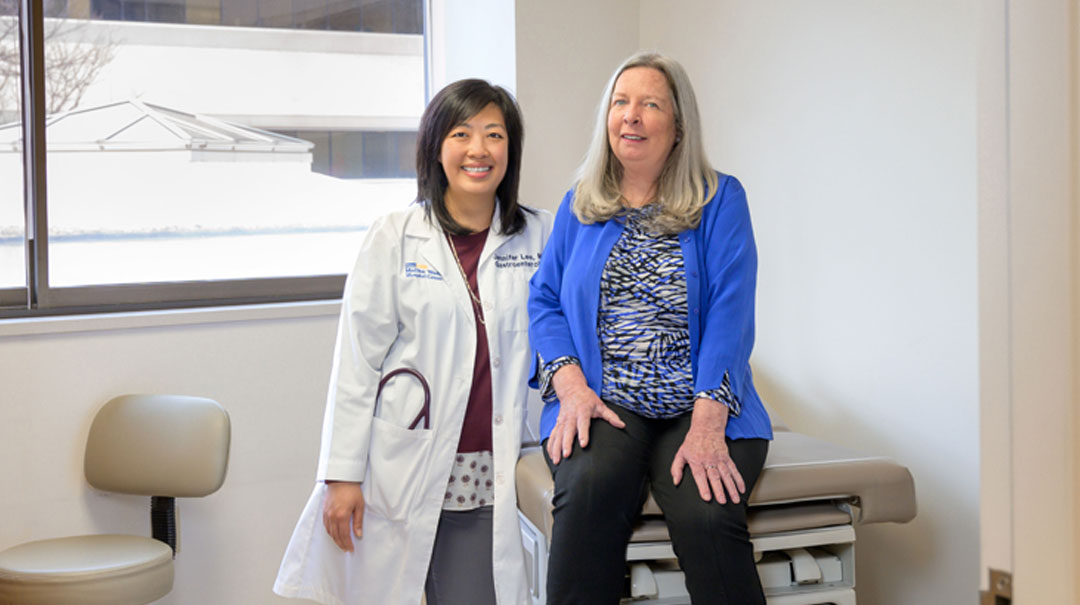
March 17, 2020Women are good at so many things, including placing others’ priorities ahead of our own. Unfortunately, this can have serious consequences on our own health.At age 65, I had put off having a colonosco...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297
- 298
- 299














