Featured Blog
-
 January 16, 2026
January 16, 2026A wild flip-flop or flutter in the chest. A sense of deep, unexplained fatigue. Atrial fibrillation (AFib) could be behind these uncomfortable symptoms. AFib is the most common heart rhythm disorde...
Browse blogs by hospital
Share this
All Blogs
-
December 30, 2019
Along with the holiday festivities, December brings an opportunity to reflect on the past year, and it’s been a busy one here at MedStar Health!! Over the past 12 months, we’ve cover...
-
December 23, 2019
Eating healthy is one of the best things you can do for your health. In fact, consuming a healthy diet that prioritizes fruits, vegetables, and whole foods can reduce your risk of: Diabetes...
-
 December 12, 2019
December 12, 2019Tailgating can be one of the best parts of football season. However, between the plethora of concession stands around the stadium and the unhealthy foods your friends might bring to your tailgat...
-
 December 10, 2019
December 10, 2019Millions of people experience ankle fractures (broken ankles) each year—but not all ankle fractures are the same. In fact, an ankle fracture can range from a small avulsion fragment, to a ...
-
 December 05, 2019
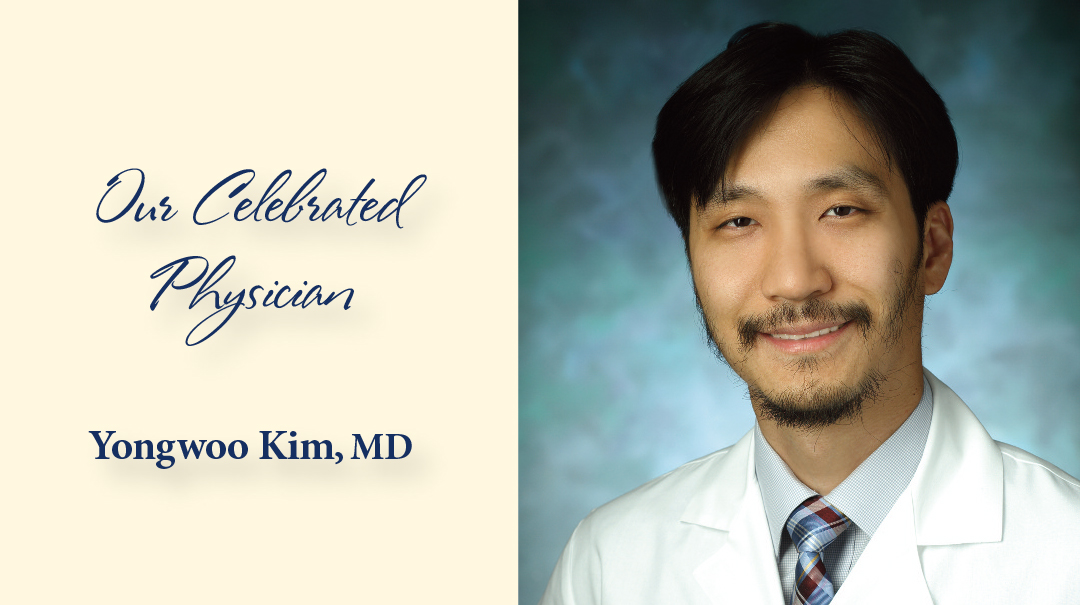
December 05, 2019As a young student in his native South Korea, Yongwoo Kim, MD, dreamed of turning his fascination with science into a career as a researcher. When he reached high school, however, those aspirations we...
-
 November 27, 2019
November 27, 2019By MedStar Team
Eating healthy is no easy feat for most people—especially during the holidays, when we have family gatherings and work events to attend. One way to combat the urge to eat unhealthy at these events is ...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296














