Featured Blog
-
 February 04, 2026
February 04, 2026Welcoming a new baby is a life-changing milestone. While preparing for a growing family can be a heartwarming time, pregnancy itself can be heart-stressing. For example, the amount of blood i...
Browse blogs by hospital
Share this
All Blogs
-
 October 05, 2017
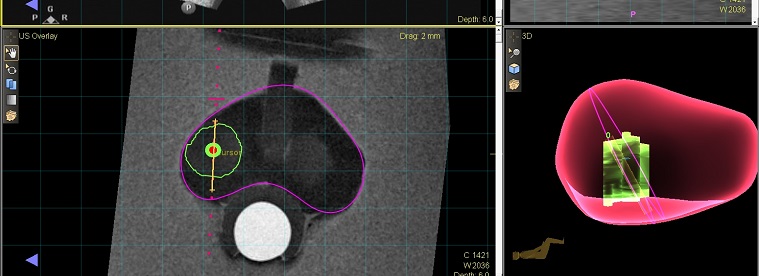
October 05, 2017Left Image: The target from an MRI is merged with an ultrasound image for targeting. Right Image: The biopsy locations are captured by the MRI-Ultrasound fusion technology. Ideally, doctors would catc...
-
 October 04, 2017
October 04, 2017(Photo L to R: Dr. Gregory Argyros, chaplains Teklu Gudeto, Emmanuel Saidi, Christopher Oranyeli, Jerome McCallum, Anthony Akinlolu, Sheila Brown, Paulette Davidson and President...
-
 October 04, 2017
October 04, 2017By Anne Gunderson, Ed.D, MS, GNP In 1999, the Institute of Medicine (IOM) released a report that estimated 44,000 to 98,000 people were dying each year in hospitals as a result of medical errors. Even...
-
 September 29, 2017
September 29, 2017By MedStar Health Research Institute
Research Grand Rounds are sponsored by MedStar Health Research Institute and Georgetown-Howard Universities Center for Clinical and Translational Science (GHUCCTS) and bring together the MedStar Heal...
-
 September 29, 2017
September 29, 2017By MedStar Health Research Institute
Open Enrollment for 2018 benefits starts next month. From October 31 to November 16, 2017, you will have the option to review your current benefit selections and determine which coverage best meets yo...
-
 September 29, 2017
September 29, 2017By MedStar Health Research Institute
On November 9, join us at the MedStar Health Research Institute (MHRI) Administrative Office at University Town Center at 8 am to learn about resources available for research at MedStar. MHRI offers a...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262














