Featured Blog
-
 February 06, 2026
February 06, 2026About half of U.S. adults—120 million of us—have high blood pressure, also called hypertension. Of these, just under 23% meet the guidelines for “controlled” blood pressure, with regular readings of ...
Browse blogs by hospital
Share this
All Blogs
-
February 07, 2021
By MedStar Team
We are MedStar Health Proud of the MedStar Plastic and Reconstructive Surgery (MPRS) department for their impressive effort in reaching over 100 publications and presentations in 2020. In 20...
-
 February 04, 2021
February 04, 2021By Mouin S. Abdallah, MD, Cardiology
Humans are warm-blooded—we maintain a steady internal body temperature, regardless of surrounding conditions. Under normal circumstances, that temperature remains at...
-
February 03, 2021
By MedStar Team
As a cardiologist, I know how important it is to eat healthy and exercise. And, up until COVID hit, I applied the same tips for a healthy heart that I recommend to my patients in my personal life. H...
-
 February 01, 2021
February 01, 2021Monti Schmitt is one of those rare individuals whose idea of fun was riding off-road over rough terrain on a motorcycle at high speeds. For the former motocross race competitor, it was natural—an...
-
January 29, 2021
As the COVID-19 vaccine becomes available across the nation, you may have some questions about whether or not you should get vaccinated. In part one of this series on frequently asked questions a...
-
 January 29, 2021
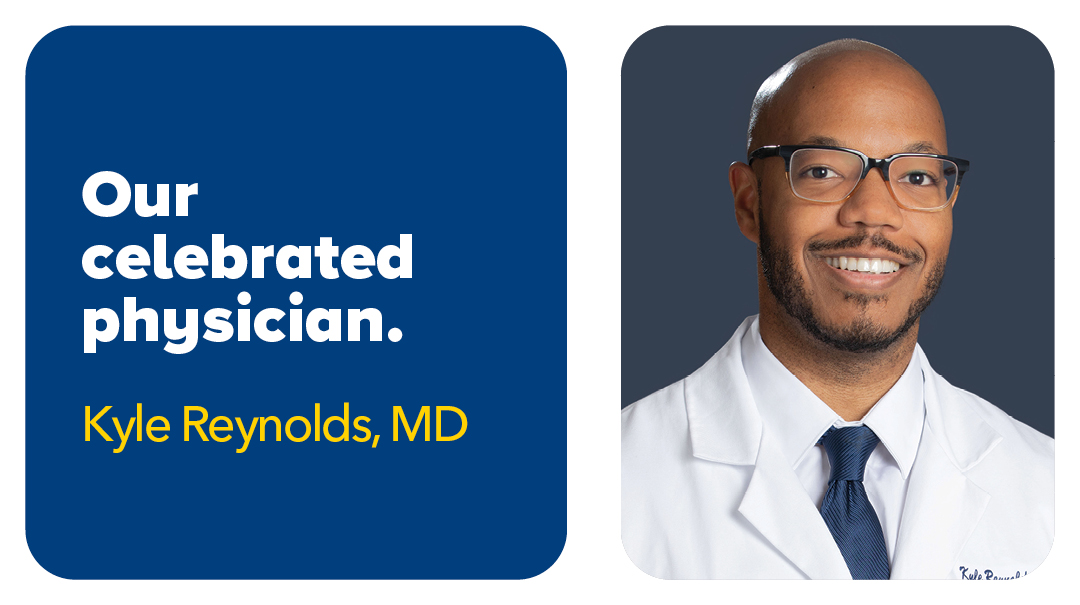
January 29, 2021As a longtime athlete, Kyle Reynolds, MD, knows that the course of a game can be altered in a heartbeat. The same holds true for his career, as the Queens, NY, native had his sights set on becomi...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297














