Featured Blog
-
 February 11, 2026
February 11, 2026Deep inside the liver, billions of protein molecules are produced every day. Sometimes, due to aging or genetic factors a particular protein, transthyretin (also known as prealbumin) can behave badly...
Browse blogs by hospital
Share this
All Blogs
-
January 09, 2019
Running a 5K is a challenging and fun way to stay fit. Although, if you aren’t careful, you can get injured while training or during the event. As 5Ks become more and more popular, we&rsq...
-
 January 08, 2019
January 08, 2019A vasectomy is one way men can prevent their partners from becoming pregnant—without affecting sexual function or the ability to orgasm. A vasectomy is a noninvasive surgery that prohibits sper...
-
 January 07, 2019
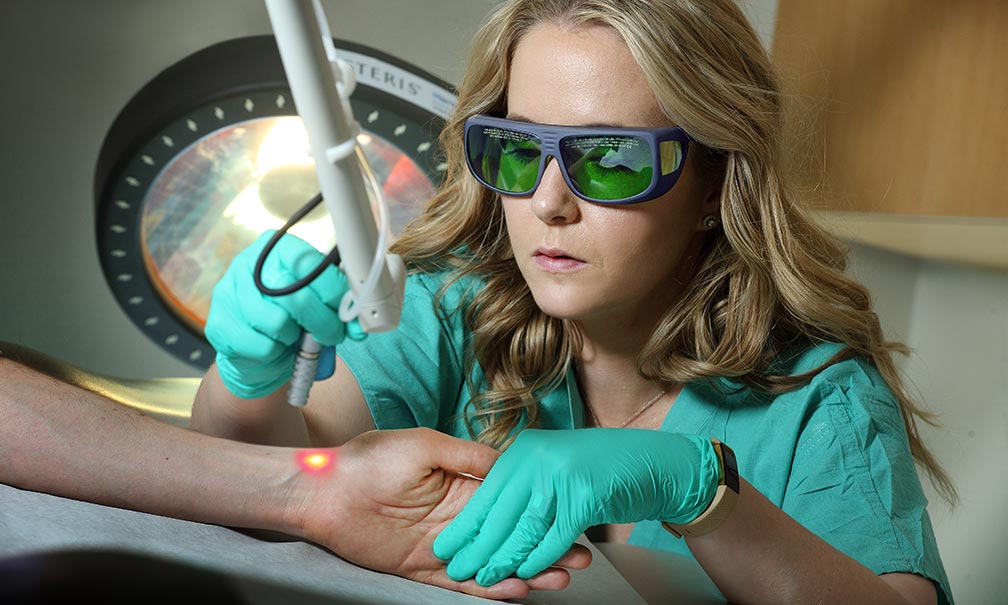
January 07, 2019It might seem unusual at first to think of a doctor using laser therapy to treat a burn injury scar. Why would burning the body’s tissue further help a patient heal? But lasers are an extremely valuab...
-
 January 04, 2019
January 04, 2019By MedStar Health Research Institute
This presentation will discuss the recent scientific advances that affected the results of the 2018 cyclosporiasis outbreak investigations and the scientific gaps that remain major public health and r...
-
 January 04, 2019
January 04, 2019By MedStar Health Research Institute
Congratulations to all MedStar researchers who had articles published in December 2018. The selected articles and link to PubMed provided below represent the body of work completed by MedStar Health i...
-
 January 04, 2019
January 04, 2019By MedStar Health Research Institute
We are pleased to announce the 2019-2021 cohorts of the MedStar Health Research and Teaching Scholars! The MedStar Research Scholars program supports the development of MedStar clinici...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297














