Featured Blog
-
 March 06, 2026
March 06, 2026The liver is your largest internal organ, and it performs a range of vital functions, including: Filtering and cleaning your blood of waste products and toxins. Creating bile, ...
Browse blogs by hospital
Share this
All Blogs
-
 October 04, 2019
October 04, 2019By MedStar Health Research Institute
At MedStar Health, patient safety is our highest priority. The most effective way to reduce the risk of contracting influenza (flu) is to get vaccinated. Even if you received a vaccination last season...
-
 October 04, 2019
October 04, 2019By MedStar Health Research Institute
Research Grand Rounds are sponsored by MedStar Health Research Institute and Georgetown-Howard Universities Center for Clinical and Translational Science (GHUCCTS) and bring together the MedStar Healt...
-
 October 04, 2019
October 04, 2019Open Enrollment for 2020 benefits starts this month. This is your opportunity to choose benefits for you and your family. From October 28 through November 18, you will have the option to review your c...
-
 October 03, 2019
October 03, 2019By MedStar Health Research Institute
MedStar Health Research Institute regularly updates, revises and creates new policies for the operational efficiency of MHRI. This month, the following policies were established or updated. MedStar He...
-
 October 02, 2019
October 02, 2019As a physician, one of the most rewarding experiences for me is to see our trauma patients recover from their complex injuries. Fortunately, this happens often at MedStar Washington Hospital Center, ...
-
 September 27, 2019
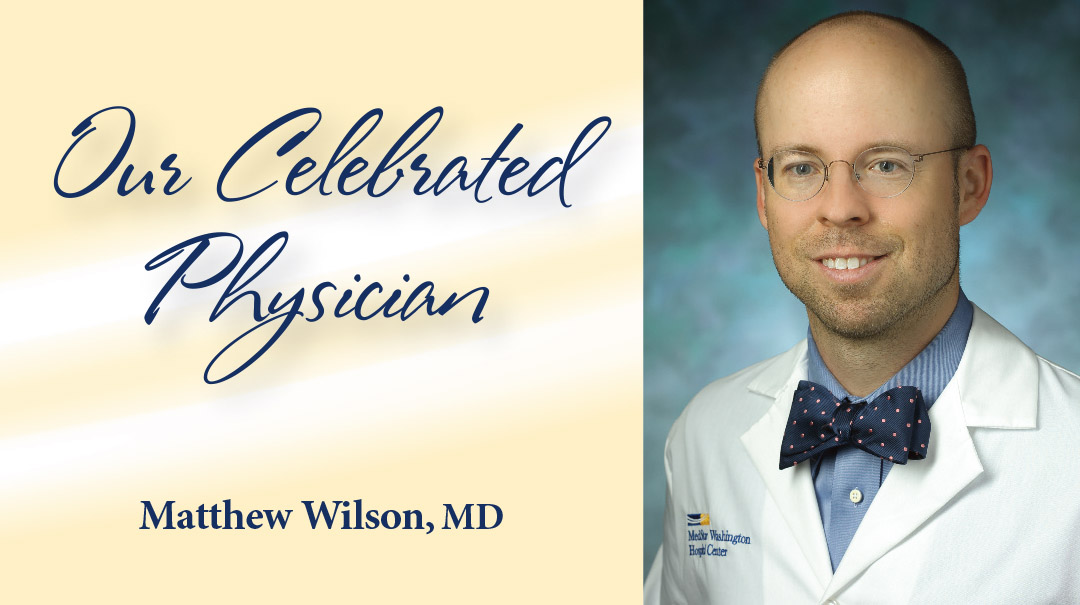
September 27, 2019Few environments may seem more different than a hectic emergency room and a quiet mountain trail. But Matthew Wilson, MD, feels right at home in both. As vice chair of Emergency Medicine at MedStar Wa...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297
- 298
- 299














