Featured Blog
-
 February 04, 2026
February 04, 2026Welcoming a new baby is a life-changing milestone. While preparing for a growing family can be a heartwarming time, pregnancy itself can be heart-stressing. For example, the amount of blood i...
Browse blogs by hospital
Share this
All Blogs
-
October 16, 2017
Nearly every pregnant woman hopes that the obstetrician she saw during her pregnancy will be the one to deliver her baby when the big day comes. And in some cases, that’s exactly wh...
-
October 16, 2017
Women who have a mastectomy often are concerned with how their breast will look and feel after reconstructive surgery. About 80 percent of women choose to get a breast implant after having breas...
-
 October 16, 2017
October 16, 2017Reena Ardeshna, MD The newest physician to join the Behavioral Health team, Dr. Ardeshna has a wide range of experience in treating various anxiety disorders, bipolar disorder, depression, schizophren...
-
 October 16, 2017
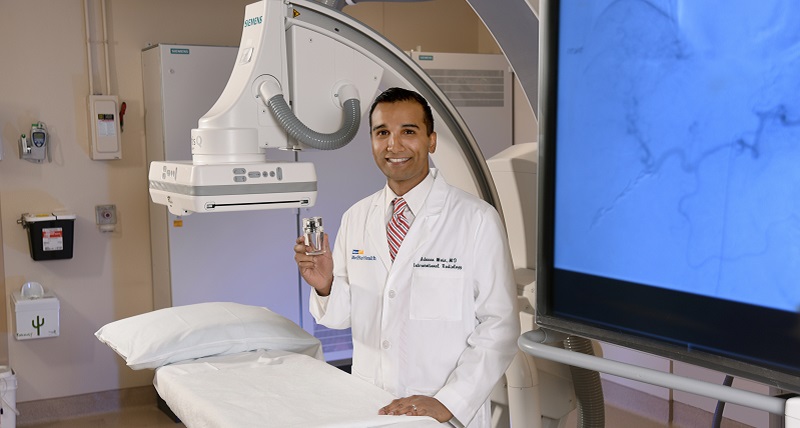
October 16, 2017Patients with Advanced Liver Cancer Among Those Benefitting Dr. Moin is one of the few specialists in the region performing Y-90 radioembolization. Advances in medicine have created a wide range of n...
-
 October 16, 2017
October 16, 2017Millions of people get a flu vaccine in the fall as recommended by the Centers for Disease Control and Prevention (CDC), the American Medical Association and other professional medical groups. But ma...
-
 October 12, 2017
October 12, 2017Some women have to deal with unpleasant body issues every day. A common one is peeing when you sneeze, cough, laugh hard or exercise, otherwise known as stress urinary incontinence. This type of bladd...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297
















