Featured Blog
-
 February 11, 2026
February 11, 2026Deep inside the liver, billions of protein molecules are produced every day. Sometimes, due to aging or genetic factors a particular protein, transthyretin (also known as prealbumin) can behave badly...
Browse blogs by hospital
Share this
All Blogs
-
 October 04, 2019
October 04, 2019By MedStar Health Research Institute
MedStar Health strives to provide associates with the tools and learning opportunities to succeed in the ever-changing healthcare industry. To accomplish this, associates are encouraged to take advant...
-
 October 03, 2019
October 03, 2019By MedStar Health Research Institute
MedStar Health Research Institute regularly updates, revises and creates new policies for the operational efficiency of MHRI. This month, the following policies were established or updated. MedStar He...
-
 October 02, 2019
October 02, 2019As a physician, one of the most rewarding experiences for me is to see our trauma patients recover from their complex injuries. Fortunately, this happens often at MedStar Washington Hospital Center, ...
-
September 27, 2019
By Megan E. Walling, MSPAS, PA-C
Now that MedStar eVisit is available, there are more ways than ever before to see a medical provider. However, many people still don’t know when it’s most appropriate to have an eVis...
-
 September 27, 2019
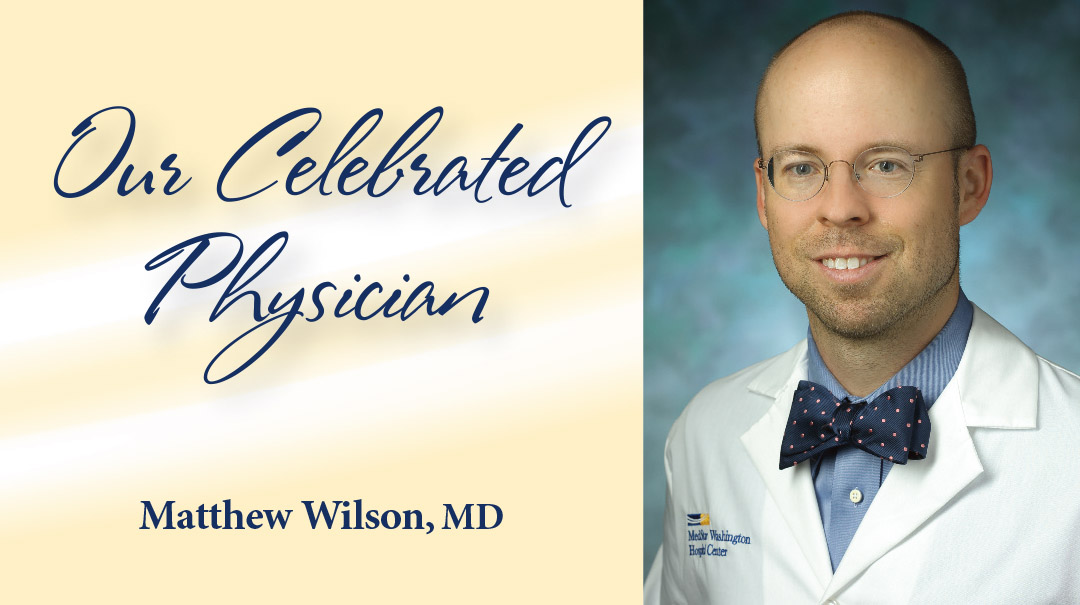
September 27, 2019Few environments may seem more different than a hectic emergency room and a quiet mountain trail. But Matthew Wilson, MD, feels right at home in both. As vice chair of Emergency Medicine at MedStar Wa...
-
 September 20, 2019
September 20, 2019The ketogenic (keto) diet started to gain popularity in the 1990s, but the interest has really spiked in the last couple of years. This eating pattern was originally developed and used to treat severe...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297














