Featured Blog
-
 January 28, 2026
January 28, 2026By Jennifer Ann Kanakry, MD, Director Stem Cell Transplant and Cellular Immunotherapy program
For many patients facing a blood cancer diagnosis, the journey includes familiar stops: chemotherapy, radiation, or antibody treatments. But when these traditionally effective medicines can no longer...
Browse blogs by hospital
Share this
All Blogs
-
 October 10, 2017
October 10, 2017Men or women can develop hernias. When they do, an organ or tissue can squeeze through a weak spot in a muscle wall. When surgery is called for, several options are available. A hernia is a weak spot,...
-
October 10, 2017
MedStar Harbor Hospital is pleased to introduce the two newest members of our Behavioral Health team. Jemima Kankam, MD, FAPA is a board-certified psychiatrist and a fellow of the American Psych...
-
October 10, 2017
Dr. Curl serves as assistant team physician for the Baltimore Orioles. When an athlete becomes injured, the first question their physician often hears is “how long will it be until I can get back out...
-
 October 06, 2017
October 06, 2017Madden now makes better nutritional choices thanks to the advice she received from her endocrinologist Dr. Kulkarni. Vanessa Madden suffered from type 2 diabetes for 13 years. She lived with extreme ...
-
 October 05, 2017
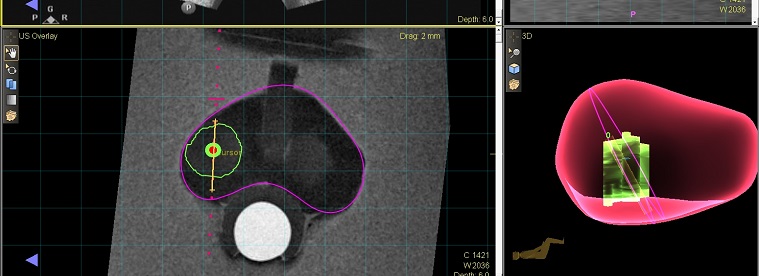
October 05, 2017Left Image: The target from an MRI is merged with an ultrasound image for targeting. Right Image: The biopsy locations are captured by the MRI-Ultrasound fusion technology. Ideally, doctors would catc...
-
 October 04, 2017
October 04, 2017(Photo L to R: Dr. Gregory Argyros, chaplains Teklu Gudeto, Emmanuel Saidi, Christopher Oranyeli, Jerome McCallum, Anthony Akinlolu, Sheila Brown, Paulette Davidson and President...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297














