Featured Blog
-
 March 06, 2026
March 06, 2026The liver is your largest internal organ, and it performs a range of vital functions, including: Filtering and cleaning your blood of waste products and toxins. Creating bile, ...
Browse blogs by hospital
Share this
All Blogs
-
 December 12, 2017MedStar Georgetown will soon offer proton therapy as part of our suite of comprehensive cancer treatments.The new proton therapy system is an innovative, highly precise form of radiation therapy.
December 12, 2017MedStar Georgetown will soon offer proton therapy as part of our suite of comprehensive cancer treatments.The new proton therapy system is an innovative, highly precise form of radiation therapy. -
 December 12, 2017Dr. Furlong discusses the risks of smoking and how lung cancer is one of the most common types of cancer. However, it is also among the most preventable.
December 12, 2017Dr. Furlong discusses the risks of smoking and how lung cancer is one of the most common types of cancer. However, it is also among the most preventable. -
 December 12, 2017
December 12, 2017Doctors are seeing more patients with thyroid cancer in the last 30 years, as data from the American Cancer Society show. Thyroid cancer is the fastest-growing cancer diagnosis in the United Sta...
-
December 11, 2017
When you see the words “plastic surgery,” your first thought probably doesn’t involve the eyes. Or you may think about cosmetic procedures to remove wrinkles or bags under the eyes.I’m an oculoplastic...
-
 December 08, 2017
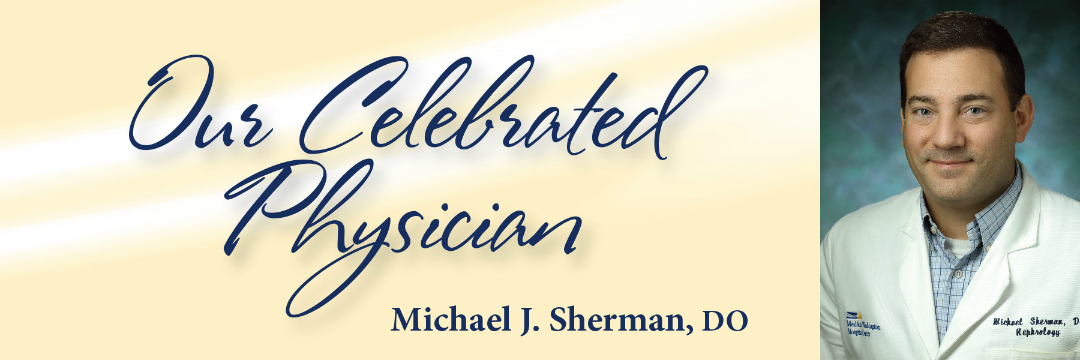
December 08, 2017Michael Sherman, DO, director of MedStar Washington Hospital Center’s Nephrology and Hypertension Clinic, says solving problems and working with people motivated his choice of a career in medicine. Ye...
-
 December 06, 2017
December 06, 2017It’s a standard part of most doctor visits: “Tell me about the medications you’re taking.” Some people quickly list a few prescriptions or pull out a list. But patients often don’t think to tell us ab...
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- 126
- 127
- 128
- 129
- 130
- 131
- 132
- 133
- 134
- 135
- 136
- 137
- 138
- 139
- 140
- 141
- 142
- 143
- 144
- 145
- 146
- 147
- 148
- 149
- 150
- 151
- 152
- 153
- 154
- 155
- 156
- 157
- 158
- 159
- 160
- 161
- 162
- 163
- 164
- 165
- 166
- 167
- 168
- 169
- 170
- 171
- 172
- 173
- 174
- 175
- 176
- 177
- 178
- 179
- 180
- 181
- 182
- 183
- 184
- 185
- 186
- 187
- 188
- 189
- 190
- 191
- 192
- 193
- 194
- 195
- 196
- 197
- 198
- 199
- 200
- 201
- 202
- 203
- 204
- 205
- 206
- 207
- 208
- 209
- 210
- 211
- 212
- 213
- 214
- 215
- 216
- 217
- 218
- 219
- 220
- 221
- 222
- 223
- 224
- 225
- 226
- 227
- 228
- 229
- 230
- 231
- 232
- 233
- 234
- 235
- 236
- 237
- 238
- 239
- 240
- 241
- 242
- 243
- 244
- 245
- 246
- 247
- 248
- 249
- 250
- 251
- 252
- 253
- 254
- 255
- 256
- 257
- 258
- 259
- 260
- 261
- 262
- 263
- 264
- 265
- 266
- 267
- 268
- 269
- 270
- 271
- 272
- 273
- 274
- 275
- 276
- 277
- 278
- 279
- 280
- 281
- 282
- 283
- 284
- 285
- 286
- 287
- 288
- 289
- 290
- 291
- 292
- 293
- 294
- 295
- 296
- 297
- 298
- 299














